Science fact sheet: Antimicrobial resistance
A growing problem
Antimicrobial resistance (AMR) is now recognized as a growing health threat to public health in Canada and around the world. AMR occurs when microbes (for example bacteria, viruses, fungi and parasites) change in ways that reduce or eliminate the effectiveness of antimicrobial drugs to treat infections by killing or slowing microbial growth.
Importance of antimicrobial drugs
Antimicrobial drugs are used to treat a wide range of infections. They are also essential for some important medical treatments. For example, antimicrobial drugs are used to prevent or control infections during chemotherapy treatment and after organ transplants, when the body's natural immune defences are lowered. Without effective antimicrobial drugs, the risk of infection would increase. The result would be prolonged illnesses and increased risk of death.
Antimicrobials are also used in livestock to treat, control and prevent bacterial disease, improve feed efficiency, promote growth, and to maintain animal health and welfare.
Overuse
Antimicrobial drugs are sometimes overused and misused in human medicine, animal medicine, the agri-food industry, and even cleaning products. Humans and animals are often exposed unintentionally (for example through environmental contamination or unsafe food) to antimicrobials or microbes that have become resistant to antimicrobials.
How does AMR develop?
Microbes naturally evolve in response to changes in their environment. This includes contact with antimicrobial drugs. The more we use antimicrobials, the faster resistance will develop. When antimicrobials are overused or misused, individual microbes that are resistant to the drug survive the treatment and multiply. Over time, enough of these resistant microbes can lead to new, drug-resistant strains that cannot be controlled by available treatments.
For example, just like any other bacteria, resistant bacteria can be spread through the food chain in uncooked meat, produce that was contaminated by water or soil, prepared food contaminated through surfaces, or in the environment through animal or human waste. They can also be spread through poor infection prevention and control in health care, or through contact between people in the community.
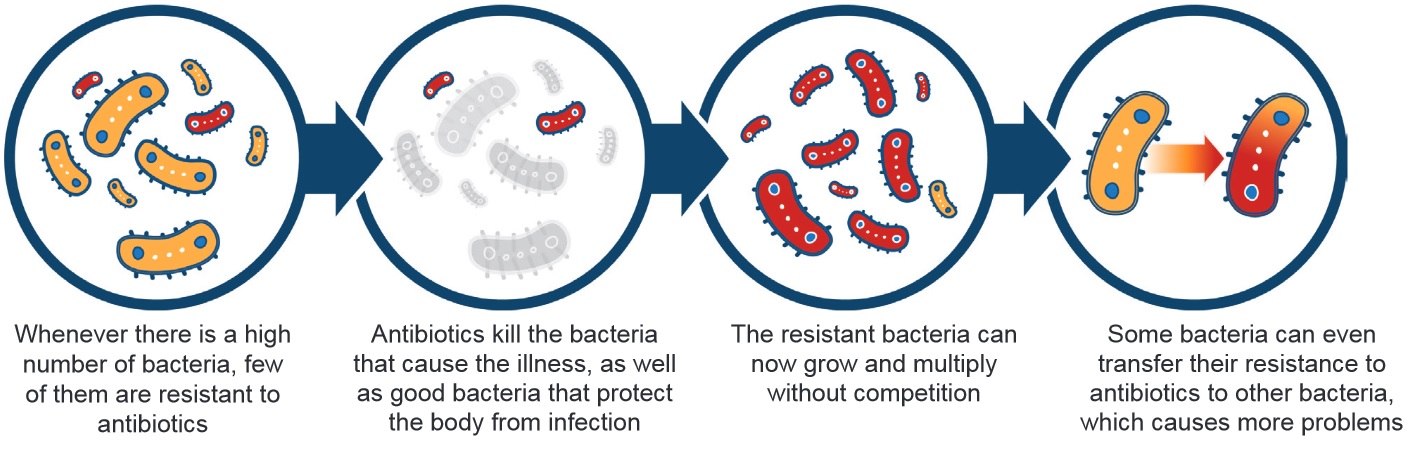
Description for image – Antimicrobial resistance
Whenever there is a high number of bacteria, a few of them are resistant to antibiotics
Antibiotics kill the bad bacteria that cause the illness, and the good bacteria that occur naturally and protect the body from infection
The resistant bacteria can now grow and multiply without competition
Some bacteria can even transfer their resistance to antibiotics to other bacteria, which causes more problems
A global threat
Public health organizations in most countries consider AMR a global threat. Antimicrobial resistant organisms (AROs) do not remain isolated in the location or environment where they first arise. Medical tourism, international food production, shipment of food and animals between countries, and travel can make it easy for AROs to travel around the world.
Antimicrobial resistance now occurs in every country around the world. In some cases, certain tested strains of E. coli bacteria show resistance that ranges from 5% to 80%. AMR is considered one of the greatest risks to human health around the world.
AMR and veterinary medicine
There is increasing evidence that antimicrobial drug use in veterinary medicine and livestock production contributes to AMR bacteria in humans. Antimicrobials are given to chickens, pigs, cattle, and other animals we eat, to treat and prevent disease. However, the spread of AROs from animals to humans makes it necessary to assess how AMR in food-producing animals puts human health at risk.
Food production and AMR in Canada
Canada is a major producer of food animals for domestic and international markets. Canada has 19 times more animals than humans, mostly poultry.
According to data published by the Canadian Integrated Program for Antimicrobial Resistance Surveillance (CIPARS), in 2015, about 1.8 million kilograms of antimicrobial drugs were distributed or sold for use in humans, animals, and crops in Canada. About 1.6 times more antimicrobials were distributed for use in animals than humans. Of these antimicrobials:
- 82% were for food producing animals
- 17% were for humans
- less than 1% were for pets
- less than 1% were for crops
Most of the antimicrobials given to animals were the same types of antimicrobial drugs used for humans. This creates a challenge as microbes develop resistance to specific antimicrobial drugs, increasing the risk to human health.
How the Government of Canada fights AMR
The Government of Canada monitors AMR in chicken, pork, and beef for E. coli, Campylobacter, and Salmonella. AMR in Campylobacter and Salmonella is also monitored in humans. This helps to measure how AROs move from animals to humans.
The CFIA uses cutting-edge technology like whole genome sequencing to analyze how resistant food-borne bacteria are to antimicrobial drugs. This technology allows scientists to look at the entire genetic structure of bacteria like E. coli or Listeria. This helps them see just how resistant certain strains are so that correction or prevention plans with food producers can be put in place.
Keeping an eye on AMR in Canada
The Public Health Agency of Canada's Canadian Antimicrobial Resistance Surveillance System (CARSS) is the focal point for reporting antimicrobial resistance and antimicrobial use.
It uses information from PHAC's surveillance systems and laboratory reference services which track resistant organisms in Canada.
CARSS works with other government departments, provincial and territorial partners, public health providers, and academia to monitor trends and impacts, and address the gaps in surveillance. The objectives of CARSS and its component programs are to:
- provide provinces, territories and stakeholders with timely and reliable data and analysis, integrating material from all of PHAC's programs and surveillance on AMR and antimicrobial use (AMU) in humans, animals and crops. This helps inform public health actions such as infection prevention and control, research, and innovation
- guide surveillance activities for resistant infections that pose the greatest risk to the health of Canadians
- provide Canadians with timely and reliable information on trends in AMR and AMU in humans and animals within Canada
- identify policies and measures that can be used to contain the emergence and spread of resistant bacteria between animals, food, and people in Canada
Working with veterinarians, feed companies, and farmers
Promoting the responsible use of antimicrobials relies on collaboration with farmers, feed companies, and veterinarians to:
- develop farm food safety programs and guidance on using antimicrobials responsibly
- fund research into other ways to improve animal health while reducing the use of antimicrobials
- change legislation to require antimicrobial use to be supervised by veterinarians
- improve the surveillance of antimicrobial use
- support programs that improve the health of farm animals and encourage animal hygiene and livestock-raising practices that reduce the need for antimicrobials
- monitor the use of authorized antimicrobials on animal farms
- educate farmers and farming communities on using antimicrobials responsibly
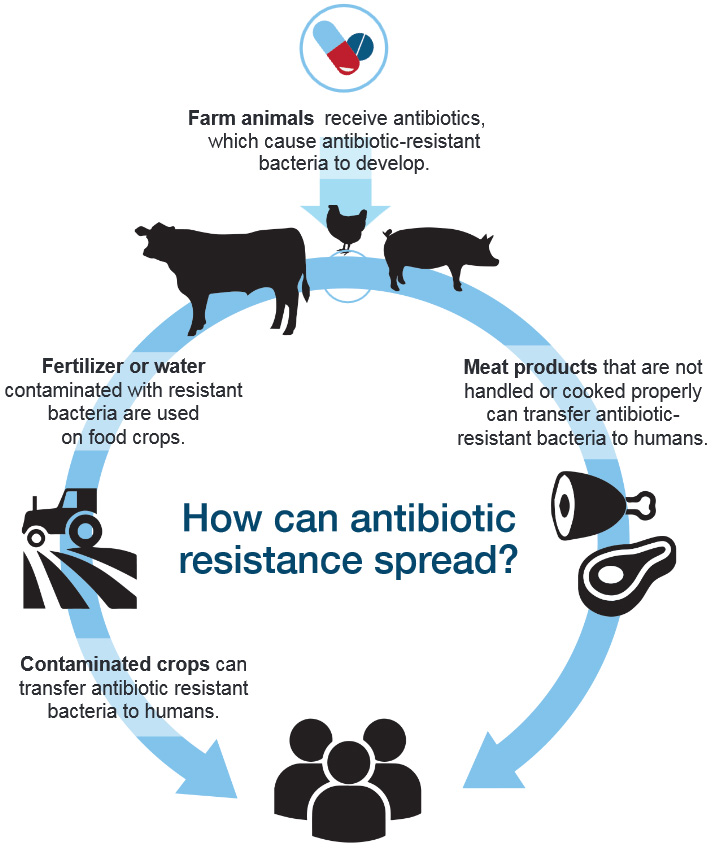
Description for image – How can antibiotic resistance spread?
Farm animals receive antibiotics, which cause antibiotic-resistant bacteria to develop.
Fertilizer or water contaminated with resistant bacteria are used on food crops.
How can antibiotic resistance spread?
Meat products that are not handled or cooked properly can transfer antibiotic-resistant bacteria to humans.
Contaminated crops can transfer antibiotic resistant bacteria to humans.
- Date modified:
