Table of Contents
- Section 1: Glossary
- Section 2: Introduction and background
- Section 3: Farm and facility specific biosecurity plan
- Section 4: Principles of infection prevention and control programs
- Section 5: Preventive horse health management program
- Section 6: New horses, returning horses, visiting horses, movements and transportation
- Section 7: Access management
- Section 8: Farm and facility management
- Section 9: Biosecurity awareness, education and training
- Section 10: Farm and facility location, design, layout and renovations to existing facilities
- Annex 1: Development of the user guide and acknowledgements
- Annex 2: Important infectious diseases of horses in Canada
- Annex 3: Self-evaluation checklist for risk assessment
- Annex 4: Conducting a horse health check
- Annex 5: Horse Health Exam Record
- Annex 6: Vitals Exam Record
- Annex 7: Sample horse event participant declaration
- Annex 8: Sample letter to participant
- Annex 9: Incoming horse protocol and checklist
- Annex 10: Additional guidance on vaccination
- Annex 11: Additional guidance on parasite control programs
- Annex 12: Important gastro-intestinal nematode parasites of horses in Canada
- Annex 13: Separating sick horses
- Annex 14: Selected disinfectants
- Annex 15: Cleaning and disinfecting procedures
Section 1: Glossary
- Access management:
-
Controlling the movement of horses, equipment, vehicles, and people on-and-off a farm or facility, as well as movement between different areas of a farm or facility to minimize the transmission of pathogens. It may include physical barriers (for example, fencing and gates that clearly indicate entry and exit points) and/or procedural measures (for example, hand washing, boot cleaning and disinfection).
- Aerosol:
-
Solid or liquid particles suspended in air that can be distributed over short distances.
- Best practices:
-
For this document a best practice is a program, process, strategy, or activity that has been shown to be most effective in preventing and controlling disease. Best practices may have to be modified before implementation to accommodate a specific farm or facility and enhance practicality.
- Bio-exclusion:
-
A set of practices to minimize the introduction of pathogens into a population of animals from an outside source.
- Bio-containment:
-
A set of practices to minimize the release of pathogens from a population of animals in a particular location (for example, a farm or facility).
- Bio-management:
-
A set of practices to minimize the transmission of pathogens within a population of animals (for example, the spread of disease among horses within a farm or facility).
- Biosecurity:
-
A set of practices used to minimize the transmission of pathogens and pests in animal and plant populations including their introduction (bio-exclusion), spread within the populations (bio-management), and release (bio-containment).
- Biosecurity zone:
-
A defined area on a farm or facility established by natural or man-made physical barriers and/or the use of biosecurity procedures designed to reduce the transmission of pathogens (for example, a controlled access zone and/or restricted access zone).
- Closed herd:
-
A population of animals that remains distinct by preventing the introduction of new animals from external sources, maintains their own breeding stock, and prevents direct contact with other herds of similar species.
- Commingle:
-
Where horses from different locations or a different health status are brought together and exposed to each other, either directly or indirectly; may be short or long term. Some examples of commingling sites include boarding stables, auctions, summer pastures, staging sites, horse shows, rodeos, 4-H events, and horse clinics.
- Controlled access point (CAP):
-
A designated and visually defined entry point to a horse farm or facility, a controlled access zone or restricted access zone to manage the traffic flow of people, horses, vehicles, equipment and materials.
- Controlled access zone (CAZ):
-
A designated area that contains the land, buildings, equipment and infrastructure involved in the care and management of horses where access and movements are controlled. Entry is restricted and managed through a controlled access point. The controlled access zone is often the first zone that is entered on a farm or facility and frequently includes laneways, equipment, storage sheds, and riding arenas, although some of these may be in the restricted access zone in other facilities. It usually excludes the house and office space of the farm owner and/or manager. The controlled access zone may include pastures and barns that horses are not currently occupying. A controlled access zone has its own specific biosecurity protocol and often encompasses the restricted access zone(s).
- Custodian:
-
Any person who has control of horses and is responsible for their care, whether on a short-term or long-term basis. This may include owners, stable owners and staff, volunteers, clients, service providers and family members.
- Disease:
-
A change from the normal state. A deviation or disruption in the structure or function of a tissue, organ or part of a living animal's body.
- Disinfection:
-
The process that is used to inactivate, decrease or eliminate pathogens from a surface or object.
- Direct contact:
-
Close physical contact between animals (for example, nose to nose, social interaction or breeding).
- Emerging disease:
-
A new infection resulting from the evolution or change of an existing pathogen or parasite resulting in a change of host range, vector, pathogenicity or strain; or the occurrence of a previously unrecognized infection or disease.
- Endemic disease:
-
The continued presence of a disease in a specific population or area usually at the same level - often a low level. In animals, it is sometimes referred to as enzootic disease.
- Event:
-
An organized gathering of horses from two or more farms or facilities for a set amount of time. A horse event or activity is defined as any market, sales or auction, fair, parade, race, horse show, meeting, recreational activity, demonstration or clinic, rodeo, competition, or any other horse gathering.
- Foreign animal disease:
-
An existing or emerging animal disease that poses a severe threat to animal health, the economy, and/or human health that is not usually present in the country.
- Facility:
-
A defined area of land and all associated buildings used primarily for the short-term care and maintenance of horses for commercial purposes and events where commingling is common (for example, competition grounds, race tracks and auction markets).
- Farm:
-
A defined area of land and all associated buildings used primarily for the long-term care and maintenance of horses (for example, boarding stables, breeding farms and riding centres).
- Federal reportable disease:
-
Refers to diseases in federal and/or provincial acts and regulations. Federally reportable diseases are outlined in the Health of Animals Act and Reportable Diseases Regulations and are usually of significant importance to human or animal health or to the Canadian economy. Animal owners, veterinarians and laboratories are required to immediately report the presence of an animal that is contaminated or suspected of being contaminated with one of these diseases to a Canadian Food Inspection Agency district veterinarian. Control or eradication measures may be applied immediately. A list of federally reportable diseases is available on the CFIA website.
- Fomite:
-
Any inanimate object or substance, such as clothing, footwear, equipment, tack, water or feed that mechanically transmits a pathogen from one individual to another.
- Health status:
-
Current state of health of the animal or herd, including both its condition and the presence of pathogens in the animal or herd. Information used to establish the health status includes the disease history and the results of any diagnostic testing, herd health management practices, vaccination and deworming protocols in sufficient detail to determine compatibility with the resident herd, and housing and movement detail sufficient to identify any potential recent disease exposure.
- Horse:
-
Refers to all domestic equine species, namely horses, ponies, miniature horses, donkeys, mules and hinnies.
- Immediately notifiable disease:
-
In general, immediately notifiable diseases are diseases exotic to Canada for which there are no control or eradication programs and are to be reported immediately to a specific government agency.
The Canadian Food Inspection Agency can undertake control measures for such diseases when notified of their presence in Canada. This category also includes some rare indigenous diseases. A herd or flock of origin must be certified as being free from these diseases in order to meet import requirements of trading partners. Some provincial ministries may require notification for surveillance and/or control of certain immediately notifiable diseases.
- Indirect contact:
-
Refers to contact with a pathogen without directly coming into contact with the source (for example, aerosol or contaminated fomites).
- Infection:
-
The invasion and multiplication or reproduction of pathogens such as bacteria, viruses, and parasites in the tissues of a living animal.
- Infectious disease:
-
Disease caused by pathogens (for example, parasites, bacteria, viruses, fungi or prions).
- Medical waste:
-
Waste generated by administration of treatments (for example, needles, syringes, expired medications, and disposable materials used in the treatment of horses).
- Mode of transmission:
-
The method whereby pathogens are transmitted from one animal or place to another. An example of direct transmission is nose-to-nose contact. Examples of indirect transmission may include contact with contaminated bodily fluids, vectors or fomites.
- Monitoring:
-
This refers to the systematic observation and recording of clinical signs that reflect the health parameters of the horse (for example, heart rate, respiratory rate, temperature, for mental status [responsive and alert], for gait and posture [normal, coordinated, not lame], for body condition [thin, normal, obese]). The level of monitoring is dependent on the health status of the horse.
- Mortality:
-
A measure of the number of deaths in a population.
- Normal carrier or subclinical carrier:
-
A horse that displays no signs of sickness but is harbouring a pathogen.
- Pathogenicity:
-
The ability or capacity of a pathogen to cause disease in a living organism.
- Pathogens:
-
Bacteria (including mycoplasma), viruses, fungi, parasites and other microorganisms that can cause disease.
- Peer group:
-
Horses of similar age (for example, yearlings), use (for example, broodmares and school horses), or health status (for example, same preventive health program).
- Personal protective equipment (PPE):
-
Refers to specialized clothing and equipment worn by an individual to provide a protective barrier against exposure and injury from hazards. It can be used to protect against pathogens, chemicals (disinfectants and medications) and physical hazards (from needles or bites), however the specifications of the equipment are different for each hazard. For infectious diseases, personal protective equipment includes coveralls, boots, boot covers, gloves, and in some instances, face shields and respirators that protect skin, mucous membranes and airways from pathogens. Personal protective equipment also reduces the transmission of pathogens to other horses from contaminated clothing, equipment and dirty hands.
- Pests:
-
Includes insects, spiders, ticks, rodents, birds and other animals that pose a nuisance to horses.
- Physical barriers:
-
The use of physical structures and items to minimize exposure to pathogens. This includes the use of fences and gates to manage access and traffic flow and solid pen partitions to minimize contact between horses. It also includes the use of protective clothing, boots and gloves that provide a barrier to contamination and/or infection of a person.
- Procedural measures:
-
The use of processes such as hand washing, cleaning and disinfection to minimize the transmission of pathogens, procedures for assessing the health status of new horses and vaccination to protect horse health.
- Provincial reportable/notifiable diseases:
-
Some provincial agriculture departments require reporting of diseases outlined in their provincial animal disease legislation. For additional information, contact the respective provincial agriculture department.
- Restricted access zone (RAZ):
-
A designated area where horses commonly reside (are stabled, housed, pastured) and where access by people, equipment and materials is further restricted. The zone(s) include the pens, barns, and pastures, as well as separation areas used for new, visiting and sick horses. The layout and management practices of individual farms and facilities will determine whether manure storage and other production infrastructure directly involved in animal care and maintenance should be included within the restricted access zone.
- Risk:
-
The likelihood of an unfavorable event occurring and affecting health.
Examples of high and low risk
- Event
- High-risk event - A horse auction/sale poses a high risk to horse health when there are no disease prevention requirements and protocols in place, and there are a high number of horses from multiple locations commingling.
- Low-risk event - An event such as the Pan-Am equine games poses a low risk to horse health where high level, healthy equine athletes are subject to strict biosecurity protocols, including testing and vaccination requirements prior to arrival, and regular monitoring by specially appointed equine veterinarians.
- Horses - Can pose a risk for spreading disease and/or be at risk of acquiring disease.
- Higher risk or high-risk horse for transmitting disease: Horses that are a higher risk for harbouring and transmitting pathogens. This includes horses that are: visibly sick (clinical infection), infected but not showing signs of sickness (subclinical infection), known to have been exposed to sick horses, and those that have recently recovered from sickness.
- Higher risk or high risk of becoming infected or sick - A young horse which has little immunity to disease and is at a higher risk of becoming infected or sick. The lack of immunity may result from not being vaccinated, being improperly vaccinated, and/or having little previous exposure to small numbers of pathogens from other horses (which may occur when raised in a closed herd). Any horse that is debilitated, stressed, malnourished, dehydrated, very young, very old, one with a long-standing or underlying health issue would be at high risk. If these horses are then exposed to a high-risk event where there is exposure to many other horses of varying health status, they may become sick.
- Lower risk or low-risk horse for transmitting disease or becoming infected or sick - Horses that are healthy, well vaccinated, well-nourished and managed under a herd health program and rarely travel or are rarely exposed to horses of different health status are a low risk or a lower risk for transmitting disease or becoming infected or sick when exposed to pathogens.
- Event
- Sanitize:
-
A process that reduces the number of pathogens without completely eliminating all microbial forms on a surface.
- Separation:
-
Using physical barriers or distance to prevent direct contact between horses. Separation is a management tool to minimize the risk of introduction and spread of disease. Other terminology such as isolation and quarantine is commonly used for specific purposes of separation
- Quarantine: A process of separating an animal(s) and restricting movement of the animal; it can be considered a "state of enforced isolation". Frequently, it is a regulatory approach to separate horses to establish and maintain a desired health status.
- Isolation: The process of separating animals that are sick, suspected to be sick, or of an unknown or lesser health status from healthy animals. The period of separation ends when animals have recovered, or been determined to be healthy, or aligned with the health status of the herd. Separation includes measures to prevent direct contact (nose-to-nose) and indirect contact (shared equipment) between isolated animals and the remainder of the herd.
- Sharps:
-
Common medical items including needles, scalpels, scissors, staples, and other objects capable of puncturing or cutting skin.
- Sharps container:
-
A container used to safely store used needles and other sharps for disposal. Only "approved" sharps containers should be used, as they are designed to prevent injuries by being puncture resistant and to prevent spillage or removal of disposed items.
- Shedding:
-
Transmission of an infectious agent from an animal to another animal or to the environment; can occur in the absence of clinical signs.
- Standard operating procedure (SOP):
-
A defined and documented procedure to be followed, detailing the steps to be taken to meet an objective. This includes any formal process that a custodian uses to define how they manage their operations on a day to day basis. The protocol may be formally documented or a non-documented process that is strictly followed. The intent is to focus on the process rather than the documentation.
- Susceptible host:
-
A person or animal who lacks the immunity or ability to resist the invasion of pathogens which then multiply or reproduce resulting in infection.
- Vector:
-
An organism such as a mosquito, fly, flea, tick, rodent, animal or person that transmits pathogens from an infected host (a horse) to another animal. A biological vector is one in which the pathogen develops or multiplies in the vector's body before becoming infective to the recipient animal. A mechanical vector is one which transmits an infective organism from one host to another but which is not essential to the life cycle of the pathogen.
- Wildlife:
-
All undomesticated animals (fauna) living freely in their natural habitat. Wildlife may come into occasional inadvertent contact with domestic horses on their farm or facility.
- Zoonotic disease:
-
A disease caused by pathogens that can occur in both animals and humans (for example, Methicillin resistant Staphylococcus aureus [MRSA] and Salmonella sp.).
Section 2: Introduction and background
Biosecurity: Cost-effective health insurance for your horse and all of Canada's horses
This biosecurity user guide supports the national biosecurity standard. It provides greater detail and practical information on specific biosecurity measures at the farm and facility level, including tools to assist horse owners and custodians in developing and implementing biosecurity. The guide is organized using the same framework as the biosecurity standard. (Refer to Annex 1 for information on development of the user guide).
Infectious diseases of horses are a common occurrence and are a reality that horse owners and custodians must face. As a horse owner or custodian, you care about and are ultimately responsible for ensuring the health and welfare of your horse(s). The choices you make (whether selecting a boarding stable, locations for riding or the competitions/events you wish to attend) affect the disease risks your horse(s) are exposed to and your ability to provide for and protect their health and well-being.
Biosecurity can manage disease risks

2.1 What is biosecurity?
Biosecurity is a set of measures used to protect horse health by reducing the spread of contagious diseases and pests.
Biosecurity is: "A set of practices used to minimize the transmission of pathogens and pests in animal and plant populations, including their introduction (bio-exclusion), spread within the populations (bio-management), and release (bio-containment)."
Good biosecurity is practiced every day, not only in the event of a disease outbreak. Biosecurity practices are difficult to "ramp-up" if not already a part of the daily routine. The level of biosecurity required often depends on the size of an operation, the venue and risks that are present. For example, biosecurity considerations at a large international show or racetrack with a large population of visiting horses are more complex than those needed at a small stable where horses seldom travel.
The threat of infectious disease is always present. Ideally, biosecurity would eliminate disease threats by preventing exposure to pathogens and their spread. Eliminating all threats is impractical and rarely achievable, therefore, at the farm level think of biosecurity as risk management.
Biosecurity requires balancing the:
- risk of disease transmission;
- consequences of disease occurring; and
- measures required to minimize disease.
As a horse owner or custodian, your tolerance for disease risk likely varies from other horse owners. Similarly, farm and facility owners and managers may have different disease risk tolerances depending on the use of their property and the clientele (boarders or participants) they may serve. It is important to recognize these different disease risk tolerances because it influences the:
- extent of the biosecurity measures that are implemented on farms and facilities; and
- willingness of horse owners and custodians to implement and comply with biosecurity measures.
Biosecurity measures need to be tailored to the needs of individual farms and facilities. The plans should be developed with the assistance of the attending veterinarian taking into account your goals, management practices, and the internal and external disease threats. Biosecurity plans must be understood, practical, achievable and sustainable. Because the consequences of disease are many and far reaching you should not look at your biosecurity practices and risk tolerance without considering the rest of the industry.
10 Biosecurity considerations for all horse owners and custodians
- Apply biosecurity every day and not just during a disease outbreak.
- Work with your veterinarian to develop an infection control plan that is right for your horse(s) and farm or facility.
- Define the biosecurity needs and take steps to reduce the risk of disease introduction and spread.
- When doing a risk assessment, consider the level of risk you are willing to tolerate on your farm, facility or property. For example, an active training stable of healthy adult horses can have very different needs than a breeding facility that houses foals at high risk for serious disease if exposed to certain pathogens. The focus of all farms and facilities should be to reduce the occurrence and impact of disease rather than complete prevention.
- Recognize that horses and humans are not the only biosecurity risk to your herd. Minimize the presence of rodents and insects by keeping feed secure and eliminating standing water.
- Vaccinate your horses against disease risks. Vaccination is one of the pillars of biosecurity, which will help in reducing the risk of infection for specific diseases.
- Do not use communal water sources or share equipment, and keep your horse(s) under your control (when around unfamiliar horses).
- Ask people to wash their hands before handling your horse for any reason.
- When transporting horses or housing them in stalls away from home, clean and disinfect stalls prior to introducing the horse to its "home away from home."
- Monitor your horse daily for clinical signs that may result from an infectious disease such as reduced appetite, depression, fever, nasal discharge, coughing, diarrhea, or acute onset of neurologic distress. Know how to take your horse's temperature and learn what their normal is (normal for adult horses can range from 37.0-38.5°C [98.6-101.3°F]). Having a baseline will help recognize when something is wrong. When in doubt, call your veterinarian!
Spot the biosecurity concerns
Everything changes over time, including the way we interact with our surroundings. We grow accustomed to our own environments and this familiarity can reduce critical observation. Issues that may be important can be overlooked: the deteriorating fence, water runoff from spring thaws and summer rains, and broken or missing equipment. It is important to critically examine the routine tasks and details on your horse farm or facility as they play a vital role in managing disease.
The following pictures depict a small horse farm with a number of biosecurity concerns that are not being managed. Before reading this guide, take some time to identify as many biosecurity issues as you can. After reading the guide, review the diagrams again to determine if there are any issues that you have missed. Answers are provided below each diagram.
Figure 1: Identify the biosecurity concerns
There are a number of biosecurity concerns on this property. How many can you identify?

Description for image – Figure 1: Identify the biosecurity concerns
a picture of a small horse farm. The horse area is located on the front portion of the property and is separated from the house which sits behind it by a wooden fence painted white. The gate to the farm is open and there is a large sign next to the gate that states: "Majestic Manes Ranch. Everyone Welcome. If you can sit you can ride." The farm is primarily grass, a few trees and in the center of the property is a small pond that extends into the property the house is on. There are multiple horses on the property. There is one horse next to the pond that is lying on its side and appears to be dead. There is a coyote standing near the front gate. There are a number of trailers and pick-up trucks scattered throughout the property in a disorderly fashion. There is a wooden horse barn on the right side, the doors to it are open and a large stack of hay bales is sitting in front of it. There are number of large metal drums stacked next to the barn as well as a large pile of manure with a pitchfork sticking out of it. There is a wheelbarrow filled with manure next to the hay bales.
Biosecurity concerns
- Access: There is little to protect horses on this farm from diseases that may be transmitted by people and equipment contaminated by pathogens and sick horses. The farm gate is not secured, the barn doors are open and no biosecurity zones or biosecurity signage is present. The farm sign encourages visitor entry and provides no guidance on what biosecurity procedures, if any, are required. No owner contact information is provided for visitors seeking guidance. There is no designated area for visitor parking; vehicles and trailers are parked in various locations in horse pasture and adjacent to the barn.
- Traffic Flow: There are no laneways or pathways onsite to manage the traffic flow of people and animals. There are no paved surfaces aside of the barn floor. Wet conditions will result in tracking mud, manure and other debris into and out of areas. It will be difficult to minimize the spread of disease without clean, hard-surfaced pathways for movements.
- Wildlife and pest control: A coyote is visible near the front of the property. There are some manure piles on the property and some barrels adjacent to the barn, and this may provide habitat for rodents, insects and other pests. Vehicles and livestock trailers may also provide secure habitat for some pests.
- Feed and water: Feed and water sources are not protected from contamination. Hay bales are stacked outside providing access to horses, other livestock and wildlife. Horses have access to pond water, which can be contaminated by wildlife, horses and runoff from manure piles.
- Manure: Manure can be a source of pathogens, can contaminate feed and water sources and can provide a breeding site for insects. Manure is improperly stored: there is a large pile adjacent to the barn and a smaller pile in the horse pasture. There is a wheelbarrow with manure in it close to the stacked hay. Ideally manure should be composted and stored to prevent access by pests, wildlife and horses.
- There is no ability to separate horses outside, no turn-out pens and only one fenced outdoor area that all horses share. One horse appears to have died and has not been properly disposed of.
Figure 2: Identify the biosecurity concerns
There are a number of biosecurity issues in this barn, look carefully and identify them.

Description for image – Figure 2: Identify the biosecurity concerns
The picture is of the inside of a small wooden horse barn with a concrete floor. In the middle of the floor is a large pile of manure, a water puddle and a number of mice or rats can be seen. There are four horse stalls; three of the stalls are on the back wall and two of the stalls contain horses. The other horse stall is on the bottom wall close to the door. There is a wash stall on the left rear wall of the barn which has a few bales of hay on the floor, a pair of boots in front of it and a bucket of water with a hose in it.
On the outside of the wash stall are some clipboards and some tools. On the ground in front of the stalls containing horses are some toolboxes and bottles of medication.
Biosecurity concerns
- Horse stalls permit direct contact with neighbouring stall mates - one horse is taking full advantage of this.
- The stall designated for sick horses (first stall on the far side) permits contact with healthy horses. The location of this stall near the entrance places it in heavy traffic flow allowing unnecessary contact and exposure to people and horses entering and exiting the barn.
- Only one of the horses has any identification information posted on the stall (Bella's Pride). Additional records are posted on a clipboard near the stall door. The horse in pen 2 has no identification or records posted.
- There are no biosecurity standard operating procedures (SOPs) posted - the clipboard is empty; however, an arena riding schedule is present. Arena schedules are a good biosecurity practice as they can help to minimize interactions between horses; however, it likely offers little benefit on this site.
- Pooling water is present and manure is piled in the alleyway of the barn. These are attractants for pests and can be a source of pathogens. Horses can be exposed when being moved from their stalls and by owners or custodians walking through the barn and into horse stalls. Pests are present - rodents are visible near the manure pile and wash stall.
- Hay is improperly stored on the floor of the wash stall, preventing use of the stall and allowing contamination of the feed. Feed also serves as an attractant for rodents.
- Horse medications and materials are improperly stored and left on the floor of the barn outside the stalls. Not only does this increase the opportunity for them to be contaminated, it may affect their efficacy and it poses a safety hazard for pets and children.
- The hose submerged in the water bucket can become contaminated if the bucket belongs to a sick horse. Disease can then be spread to other horses when filling their water buckets.
- A pair of rubber boots is present which is a good biosecurity practice; however, no other outer clothing/cover-ups/coveralls are present.
- Doors to the barn are open, which may present a risk for access.
2.2 Why is equine biosecurity important?
Infectious disease in horses continues to rank as one of the major challenges to the equine industry, leading to sickness (and potentially death), financial costs, welfare concerns and potential risks to human health. Measures to reduce the occurrence and severity of disease in the Canadian herd are important as disease risks change locally and globally.
Goals of the user guide: To assist horse owners and custodians in protecting the health and welfare of their horses by supporting the implementation of biosecurity on all horse farms and facilities in Canada.
Goals of the national standard:
- To assist horse owners and custodians in protecting the health and welfare of their horses by minimizing the transmission of contagious diseases and reducing the frequency and severity of disease if infection occurs.
- To achieve a Canadian national herd that has a high health status with horses in good condition, with strong immunity to pathogens and an overall decrease in the number of pathogens.
- To maintain a country that is eligible to export horses worldwide.

The impacts of infectious disease in horses are significant and can be devastating. Disease can range from mild sickness to death, from occasional cases to extensive disease outbreaks. Even mild disease can result in permanent damage and impaired function. Farms and facilities with poor biosecurity may become a significant risk to the rest of the industry. It is important that every horse farm and facility develops and implements a biosecurity plan.
Some equine diseases can spread quickly, particularly in populations of horses that have never been exposed or developed resistance to the disease. An example of the rapid spread of disease is equine flu in Australia. In North America, equine influenza (equine flu), a contagious viral respiratory disease, is relatively common and vaccination is used to help protect the horse population. However, in August 2007, a serious outbreak equine flu occurred in Australia, a country previously free of the disease, following the importation of an infected stallion. The virus rapidly spread into the horse population; over 70,000 horses were infected on approximately 9000 premises.Footnote 1 Conservative estimates of the costs incurred by the Australian Government to eradicate the disease were in excess of $342 million.Footnote 2 The movement restrictions imposed on horses resulted in the cancelation of hundreds of horse events, financial hardship and impacts to human health, including psychological distress.
Equine herpesvirus (EHV1) infection in horses can result in respiratory disease and fever, neonatal foal infections, abortions in mares and neurologic disease referred to as equine herpesvirus myeloencephalopathy. In April and May 2011, a large outbreak of equine herpesvirus in Utah at a national event resulted in approximately 90 confirmed cases of equine herpesvirus and equine herpesvirus myeloencephalopathy in 10 states.Footnote 3 Over 2000 horses were deemed exposed (either at the event or from a horse that attended the event) and 13 horses either died or were euthanized.Footnote 4 In Western Canada, 17 horses in 3 provinces were infected with the neurologic form of the disease.

In recent years, outbreaks of vesicular stomatitis virus, a contagious viral disease of equines, cattle, pigs and camels have occurred in the United States. Infected animals can develop blisters that swell and rupture, resulting in sloughing of the skin in their mouth, on their tongue and less frequently their muzzle, ears, teats and above their hooves. There is no vaccine and disease prevention relies on implementing effective biosecurity measures. In an outbreak that occurred in 2014 and 2015, 647 animals distributed over 435 premises in 4 US states were infected.Footnote 5 Another US outbreak in 2015 and 2016 affected 823 premises in 8 states.Footnote 6 Vesicular stomatitis is a federally reportable disease and outbreaks result in local and international movement restrictions and economic losses. Fortunately, Canada has remained free of vesicular stomatitis, the last outbreak occurring in 1949.
The significance of these disease outbreaks emphasizes the importance of developing and implementing biosecurity measures at the interface of all levels of horse contact and movement-from the biosecurity measures used in the daily care of your horse to those required when moving horses internationally.
Figure 3: Your horse - Part of a larger herd

Description for flowchart – Figure 3: Your horse - Part of a larger herd
The diagram consists of 5 circles that are different sizes and are layered around each other. Each circle represents a different aspect of the industry. Each circle contains text inside it. Beginning at the bottom with the smallest circle, the text inside the circles states: Individual Horse. The second circle states: Your Herd. The third circle states: Your Farm or Facility. The four circle states: Provincial and National Herds. The fifth and largest circle that contains all of the four other circles states: International Trade and Movement Agreements, International Herd.
This diagram illustrates the relationship of an individual horse to the national and international horse industry. It emphasizes the impact that disease left uncontrolled from an individual horse can have on the horse industry in Canada. Modified from Equine Biosecurity Principles and Best Practices: Disease Transmission; Government of Alberta.
2.3 Who is this document for?
Biosecurity is a shared responsibility that everyone in the horse industry must participate in. If you are responsible for a horse facility or the owner or custodian of horses, you share the responsibility to respect and implement appropriate biosecurity practices. As a horse owner or custodian, you are ultimately responsible for the health and welfare of your horse(s) and the level of disease risk you are willing to accept is a choice you must make. If biosecurity risks are unacceptable at a particular facility, you can either relocate horses (if boarding) or choose not to attend a particular event.
The guidance in the document is primarily for horse custodians, those individuals directly responsible for the care of horses or who have influence on those directly responsible.
One approach some horse owners and custodians take to minimize disease risks is to maintain a "closed herd" by eliminating the movement of horses onto and off of the property. While this may be feasible on some properties and can reduce disease risks, it does not eliminate disease risks posed by pathogens transmitted by biological and mechanical vectors such as mosquitoes, flies, ticks, feed, people, and tack or equipment.
2.4 What is the purpose of this guide?
The national biosecurity standard established a set of guidelines and recommendations to assist you in developing a biosecurity plan to minimize the risk of disease to your horse(s) or horse(s) you are responsible for. This user guide provides additional details and tools to achieve and implement the biosecurity elements in the standard. This will help keep disease out of your herd and neighbouring herds.
Be a good neighbour - Practice biosecurity to prevent the spread of disease.
2.5 Organization of the guide
The guide mirrors the organization of the standard and consists of seven biosecurity components that comprise a comprehensive on-farm or facility biosecurity program:
- Developing your biosecurity plan: Self-evaluation assessment checklist
- Monitoring and maintaining animal health and disease response
- New horses, returning horses, visiting horses, movements and transportation
- Access management
- Farm and facility management
- Biosecurity awareness, education and training
- Farm and facility location, design, layout and renovations to existing facilities
For each biosecurity component, a broad goal is established which is supported by a number of best practices to provide the overall direction for reducing disease transmission risks. If you own a single horse that rarely leaves an isolated property, you face different biosecurity challenges than horse owners or custodians and managers at a busy boarding facility or race track. Some components of biosecurity recommendations are divided into two groups: small farms and facilities and large facilities (which include, but are not limited to, event facilities and race tracks).
Section 3: Farm and facility specific biosecurity plan
Biosecurity: Keeping your horse(s) healthy and safe
3.1 Developing your farm or facility biosecurity plan
Developing a farm or facility biosecurity plan involves achieving the right balance between disease risk and prevention. While you and other horse owners and custodians may identify and implement similar biosecurity measures, each biosecurity plan is unique as it addresses the risks to your farm or facility.
It is helpful to have a basic understanding of the diseases that are most likely to pose a risk to your horse, (Refer to Annex 2) how these diseases are transmitted and methods of protecting your horse from disease. Work with your farm or facility veterinarian and industry experts on developing a plan.
Step 1: Prepare a diagram of the farm or facility
A farm or facility diagram is useful for visualizing and identifying opportunities for horses to come into contact with other animals, people and equipment that are potential sources of disease.
Create a diagram of the premises and identify:
- property boundaries, fences and gates;
- location of neighbouring properties with horses or livestock;
- laneways, pathways, parking locations and traffic routes;
- pasture, animal housing, arena and eventing areas;
- storage locations for bedding, feed, manure and garbage;
- water sources, watering and feeding locations; and
- other areas on the site where people, horses and equipment may come into contact.
Review the diagram and create a list of the biosecurity concerns.
Step 2: Identify the risks - What diseases are concerns and how are they transmitted?
Diseases present in the local horse population and diseases that have previously occurred on the property are of primary importance. If you are travelling with your horse(s), consider disease risks from geographic areas you travel to. Talk to your neighbours that own horses, the clubs or associations you ride with, and your veterinarian to determine the status of local diseases.
Step 3: Review management practices and complete the self-assessment tool
Most horse care and management practices pose a risk for introducing and spreading disease. The biosecurity risks increase at a facility when there are additional people and horses with increased movement both on and off the farm or facility and around the property. Identify your daily care and management practices and any less frequent activities (for example, visits of non-resident horses to the property and resident horses returning after commingling with other horses) that might result in transmitting disease. Review your farm or facility diagram to help with this step.
Complete the biosecurity self-assessment tool using the information and biosecurity concerns identified in Steps 1 and 2 and the management practices identified above. (Refer to Annex 3 self-assessment tool). It is organized based on the seven components of a biosecurity plan.
When completed, review the self-assessment and identify areas where biosecurity practices are being effectively managed and those where improvements can be made.
Step 4: Identify biosecurity goals and best practices
From the review of the self-assessment tool and farm or facility diagram, identify the biosecurity challenges and risks. Using the biosecurity standard and user guide, identify biosecurity goals and best practices that can be implemented to address the biosecurity gaps. Discuss the strategies with your veterinarian and other sources of biosecurity expertise (provincial government livestock and extension specialists, industry associations, and universities) as necessary.
Step 5: Develop an implementation strategy
While all biosecurity risks need to be addressed, some will be more critical than others. Prioritize the biosecurity tasks and establish a timeline for their completion.
Establish short term goals and activities. These:
- can be planned and implemented within 12 months;
- are aligned to the current objectives and goals of your farm or facility; and
- often require minimal investment of time and capital.
Establish long-term activities. These can:
- be planned and implemented over more than one year;
- require changes in the physical infrastructure or layout of the farm or facility;
- require additional financial or personnel resources that are not currently available; and
- expand the overall goals and objectives of your management plan beyond their current scope.
Step 6: Review the effectiveness of the biosecurity plan and seek continuous improvement
The effectiveness of the biosecurity plan is measured by the adoption of its biosecurity practices, their integration into daily routines and the impact to the health status of horses on the property. When necessary, design and implement improvements to the biosecurity plan.
- assess the applicability and effectiveness of the biosecurity practices by reviewing key health performance indicators contained in the herd health records (see section 5.0) during and following implementation of the biosecurity plan and as changes to the plan are made;
- consult with your veterinarian and other advisors on biosecurity and adjust your plan as necessary;
- meet with family, staff, boarders and anyone with unrestricted access to the farm or facility at least twice yearly and following the implementation of a new practice to discuss the feasibility and effectiveness of each of the practices in your biosecurity plan; and
- review education and training sessions to identify areas for improvement.
3.2 Cover your bases - Biosecurity: A cycle of activities
The implementation of biosecurity principles on a farm or facility can be viewed as a cycle of activities which includes:
- Assessing the biosecurity risks;
- Developing a plan that addresses the risks;
- Implementing biosecurity measures and procedures;
- Monitoring horse health, keeping records of sicknesses and treatments, and gathering disease and pest information to evaluate the plan and identify new risks; and
- Reassessing the risks and responses on an on-going basis to ensure continuous improvement.
Figure 4: Cycle of biosecurity activities

Description for flowchart – Figure 4: Cycle of biosecurity activities
Figure 4 is an illustration of the cycle of activities that should be completed to develop and implement a biosecurity plan. The cycle of biosecurity activities has four items in the centre with arrows pointing between them in clockwise direction. The first item at the top of the cycle is Assess. Moving clockwise, the second item is Plan, the third item is Implement and the fourth item is Monitor. There is a text box by each of these items in the cycle (four in total). Above the word Assess there is a box with the following text: Identify and evaluate on an on-going basis the risks posed by diseases and pests that are a threat to your farm or facility. To the right of the word Plan there is a box with the following text inside: Develop a written biosecurity plan to address the risks - this allows for the regular review and update, facilitates continuous improvement within the farm or facility and forms the basis for training. Below he word Implement is a text box with the following text inside: Implement the biosecurity measures that were identified in the plan to address the disease and pest risks. To the left of the word Monitor is a text box with the following text: Develop and implement a surveillance program for ongoing monitoring of disease to evaluate the plan and the early detection and identification of disease.
Assess: The risks posed by the introduction of pests and diseases that threaten horse health on your farm or facility are identified and evaluated in consideration of the seven components of a biosecurity plan. The identification and evaluation of risks will allow for current biosecurity issues within a farm or facility to be addressed.
Plan and Implement: A written on-farm or facility biosecurity plan is highly recommended, regardless of the size or type of facility. A written plan allows for regular review and update, facilitates continuous improvement within the operation, and forms the base for training.
Monitor and reassess: It is important that the design, effectiveness and implementation of a biosecurity plan be assessed not only on a routine basis, but also when changes in farm practices or biosecurity issues occur. Production practices should be reviewed frequently to ensure that implemented measures are effective in relation to pest and disease prevention and control.
Additional resources on developing a biosecurity plan
- Australia Horse Venue Biosecurity Workbook and Toolkit
- Equine Guelph
- Equine Biosecurity Policies and Best Practices book - Alberta Equestrian Federation (AEF) and the Alberta Veterinary Medical Association (ABVMA)
- Horse Biosecurity Guidebook - Saskatchewan Horse Federation and Saskatchewan Ministry of Agriculture
- Biosecurity Toolkit for Equine Events - California Department of Food and Agriculture
Section 4: Principles of infection prevention and control programs
Infectious diseases in horses result from a complex interaction of three factors referred to as the disease triad:
- a horse that is susceptible to disease (the host);
- a pathogen such a bacterium, virus, fungus or parasite capable of causing disease (the agent);
- an opportunity for the host and agent to come into contact (the environment - which includes other horses and animals, the facility, food, water, soil, insects, equipment and humans).
Figure 5: The disease triad

Description for image – Figure 5: The disease triad
The diagram consists of a set of three overlapping circles of different colors. One circle contains the text host, one circle contains the text environment and one circle contains the text Agent. At the centre of the three intersecting circles is a yellow triangle with a yellow line on top representing a balance.
The disease triad illustrates that disease may result from the interaction of a susceptible horse (the host), a pathogen (the disease agent), and an environment favourable for disease development. There are many factors that influence whether disease will occur including the health of the animal, adequate nutrition, external stressors, the number of pathogens present and the ability of the pathogen to cause disease. However, there is a tipping point when sufficient factors overwhelm the ability of the animal to resist infection, tipping the balance in favor of the pathogen, which may allow disease to occur. Understanding the elements necessary for disease to occur provides the ability to influence and manage their impact to reduce disease. (Refer to Annex 2 and Annex 12 for information on equine diseases and parasites)
When discussing infection prevention, it is helpful to understand the distinction between infection and disease. Infection is the result of a pathogen invading and reproducing in a susceptible host. This does not always have an impact on the horse. Infection may lead to disease if there is a change from the normal function (for example damage to or a change in function of tissues and organs).
There are many host, agent and environmental variables that influence whether a horse will become diseased. Infection prevention and control programs rely on approaches that target these factors.
4.1 Sources of pathogens
- Horses that are infected but not showing signs of disease (a subclinical inapparent carrier or horse that has recovered from disease but still harbours the pathogen)
- Diseased horses
- Other domestic animals including pets
- Humans
- Food, water, and soil
- Equipment and other items (fomites)
- Housing areas and immediate surroundings
- Wildlife
- Pests (insects, spiders, ticks, rodents, birds and other animals that pose a nuisance to horses)


4.2 Methods of transmission
Pathogens can be transmitted (spread/transferred) by a number of routes; however, not all pathogens are transmitted by all routes. Pathogen characteristics, such as the ability to survive in the environment, can affect the mode of transmission.
- Direct transmission - Pathogens transmitted between animals through close physical contact.
- Direct contact - transmission through close physical contact between a susceptible animal and an infected animal, their bodily fluids or tissues. Depending on the pathogen, contact with skin, blood, saliva, respiratory fluids, urine, semen, fecal material and milk may result in transmission. In addition to the obvious modes of contact between individuals and groups, nose-to-nose contact over fences should always be considered.
- Indirect transmission - Some pathogens can be transmitted through an intermediate that has been contaminated and/or infected. This may be an inanimate object (a bridle, dirty clothing, contaminated feed and/or water) or a live animal (insect, rodent).
- Indirect contact - transmission through contact with people (for example, contaminated clothing, footwear, and/or hands), or with an inanimate object (fomite) through the shared use of equipment such as needles, syringes, artificial vaginas, dentistry equipment, contaminated vehicles, trailers, water buckets, and blankets. Pathogen transmission can occur over short distances (between animals on the same premises) and long distances (following travel to events and venues). Indirect contact with contaminated surfaces (dirty stalls and pens previously occupied by infected horses) can result in the transmission of pathogens. Pathogens transmitted by this route must be able to survive in the environment for the time required to come into contact with a susceptible horse.
- Ingestion - transmission by consuming feed and water contaminated by pathogens. The source of the contamination can include manure, urine, nasal discharge, and grass contaminated with parasite larvae.
- Aerosol transmission within a droplet - pathogens transmitted short distances by large fluid droplets generated by coughing, sneezing snorting and whinnying. Inhalation of these droplets can result in disease transmission.
- Airborne - transmission by very small particles that can be generated by disturbing contaminated materials. These can remain suspended in the air and travel over long distances.
- Vectors (living organisms) - transmission by a living organism (for example, people, animals, insects and ticks) infected with or contaminated by pathogens. In some instances, the insect vector is required for the development or multiplication of the pathogen prior to the pathogen being infective in the horse.
Figure 6: The status and spectrum of disease outcomes

Description for image – Figure 6: The status and spectrum of disease outcomes
The diagram provides a visual depiction of the outcomes of exposunnnnnre to disease and or status of disease in horses. There are four rows to the diagram. In the top row from left to right is a box with the text "exposure status", an oval with the text "unexposed" and an oval with the text "exposed". Two arrows point from the oval with the word "exposed" to ovals in the row below it. On the far left of the second row is a box with the text "infection status". To the right of this is an oval with the text "uninfected" and to the right of this an oval with the text "infected" . From the box reading infected are two arrows pointing to the third row. On the far left of the third row is a box with the text "disease status". To the right of this are two ovals. The first oval contains the text "subclinical (inapparent) and the second oval contains the text "Clinical (apparent). There is a two headed arrow between the two ovals. From the oval "clinical apparent" are arrows pointing to 3 boxes below it that contain the text "mild", "moderate" and "severe". There are two headed arrows between the boxes "mild" and "moderate" and between "moderate" and "severe". The last row starting on the left contains a box with the text "Outcome". To the right of this are 3 rectangles. The first rectangle contains the text "recovered", the second rectangle contains the text "disability" and the third rectangle contains the text "death". The rectangle "recovered" has arrows coming to it from the rectangles "mild", "moderate", and "severe". The rectangle "disability" has arrows coming to it from "moderate" and "severe" and the rectangle "death" has an arrow coming to it from the rectangle "severe". The rectangles with the text "recovered" and disability have a dashed box around them with dashed arrows pointing back up to the oval with the text "subclinical inapparent" and the oval with the text "uninfected" There is also a dashed arrow from the oval with the text "subclinical inapparent" to the oval with the text "uninfected".
Figure 6: illustrates the status and outcome of an individual horse or a group of horses following disease exposure. When an individual horse or group of horses are exposed to a pathogen, many factors (for example, genetics, age, health status, and the type of pathogen) influence the outcome of the exposure. Healthy horses with a robust immune system may not become infected following exposure, others may become sub-clinically infected, and some horses may develop clinical sickness and never fully recover. Horses that have been clinically infected (visible signs of sickness) may go on to become subclinically infected (no visible signs of sickness yet they still carry the pathogen) or clear the infection and become uninfected.
In a group of horses, the diagram represents the various stages and outcomes of exposure to a pathogen that can be encountered at any one period of time. There can be a gradient with some horses remaining uninfected while other horses are at different stages; some are only recently exposed, others are clinically sick and some already recovered. After exposure, some animals may continue to harbour the pathogen even if they have recovered from disease (for example, Streptococcus equi [strangles] or equine herpes virus-1 [rhino]).
When normal biosecurity measures fail, horses may become infected with pathogens that require treatment. Treatment should always be conducted under the consultation and supervision of a veterinarian. The veterinarian is the person best able to prescribe the right drug for the condition at the right dose for the proper duration of time to effect a proper treatment and response.
4.3 General concepts of infection prevention and control
A) Decrease exposure to pathogens: This is the most important approach; eliminating contact between animals and pathogens prevents infection and disease. If exposure occurs, horses may become sick if there are enough organisms (an infectious dose) that can bypass the horses' defence systems and then multiply to cause disease. Many of the biosecurity practices focus on reducing exposure including: separating healthy horses from horses that are sick or of unknown health status, not sharing horse equipment and tack, eliminating contact between individuals or groups over fences and stalls, and cleaning and disinfecting housing areas for horses on a routine schedule and before use by a different horse.
i)
- Separation of new arrivals - Separate new horses and horses returning to a herd (for example, following a period off the property and exposed to other horses) until their health status is determined and/or specific preventive measures are applied (for example, deworming and vaccination).
- Separation of potentially higher risk horses - Identify horses that are a higher risk for harbouring and transmitting pathogens and manage them appropriately (separate and treat) to minimize the risk. This may include horses that are: visibly sick (clinical infection), known to have been exposed to sick horses, and those that have recently recovered from a sickness. Horses that are clinically sick require separation from other horses and must be managed with additional biosecurity measures.
- Separation of susceptible horses - Separate horses that are more susceptible (young, pregnant, senior) to infection from other horses.


ii) Cleaning and disinfection (for example, barns, stalls, alleyways, and trailers) - Perform routine cleaning and disinfection to reduce the number of pathogens that are present. Ideally, all pathogens should be destroyed and removed by cleaning and disinfection; however, this can be very difficult to achieve. Therefore, the goal is to reduce the pathogen level below that which is required to cause infection.
iii) Hand hygiene - Perform hand washing, use hand sanitizers, and when necessary use clean disposable gloves (washing hands or using hand sanitizer after removal of gloves) to minimize pathogen spread.


iv) Personal protective equipment - Change clothing and use protective outerwear (boots, coveralls and gloves) to provide a barrier to the transmission of pathogens. Personal protective equipment can be used to protect the health of your horse and your own health.
v) Access control - Manage access to the property and horses to limit exposure. Minimizing contact, particularly contact with non-resident horses and their owners or custodians, reduces opportunity for disease transmission to resident animals.

vi) Traffic flow - Manage opportunities for direct and indirect contact between horses, people, equipment, vehicles trailers and other materials on the property. Fences, gates, pathways and signage can assist in keeping things where they need to be.
vii) Pest management - Minimize pests by: decreasing attractants (cleaning up spilled food and preventing pooling of water in paddocks and fields), controlling access and locations for pests to establish populations (using window and door screens in barns and removing unnecessary equipment and debris), and actively controlling pests through traps, bait and insecticides or pesticides when necessary. Insecticides and pesticides should be used with caution and according the manufacturer's recommendations as some products can be harmful to horses if over dosed, other animals, humans and the environment.
viii) Pasture management - Manage pastures to minimize the accumulation and transmission of pathogens and parasites among horses. (For additional details refer to section 8.3)
B) Decrease susceptibility to disease: The best way to decrease susceptibility is to ensure your horse has a high health status. This can be accomplished in the following ways: Providing proper nutrition, managing underlying disease, reducing stress, implementing a good parasite a control program, controlling housing conditions (for example, temperature and humidity), providing proper dental care, managing pain, and ensuring the proper use of antibiotics and other medications. There are other factors that affect a horse's susceptibility to disease that cannot be influenced to a significant degree: age, sex, genetics, and pregnancy. Develop and implement a horse health management program.
C) Increase resistance to disease: Vaccination is the primary method used to improve resistance to certain infectious diseases. Vaccines need to be given and stored according to the label directions in order to be effective. Many vaccines require two or more doses to be effective; booster vaccinations to maintain protection are often required on a yearly or more frequent basis. Unfortunately, a small number of horses may not be protected by a vaccine because they fail to generate a sufficient immune response, or the vaccine has been compromised through improper handling or administration. Additionally, a small percentage of horses may not be able to be vaccinated for health reasons. To protect these animals, it is important that the majority of horses are vaccinated to stop the spread of disease. Develop a vaccination program and vaccinate horses against diseases using a risk based approach in consultation with your veterinarian.
Titer testing - It is now possible to determine the level of antibody to several diseases by testing a blood sample from a horse. This may help determine when revaccination is necessary for some diseases.
However, while antibody titers can provide some indication of the level of immunity (protection) to a disease, it only provides one part of the picture. The level of antibody (the titer) required to provide protection is still unknown for many diseases. Additionally, other components of the immune system that are important in defending against disease, such as cell mediated immunity, are not measured.
Titer testing may be appropriate in some situations for certain diseases, however there are limitations which should be discussed with your veterinarian.
D) Treatment with medications to control an infectious disease: There are many different medications that can be used to help manage infectious disease, thus decreasing the chances of it spreading to other horses. The medications most commonly used to control bacterial infections are antibiotics. Due to the risk of infectious organisms developing resistance to the various antibiotics and potential adverse effects (for example, diarrhea), antibiotics (and other medications) should be used with discretion and only under the direction of a veterinarian.
Poor biosecurity and inappropriate or indiscriminate drug use can lead to antimicrobial resistance, which has a significant effect on human and animal health
Records management - Good recordkeeping and written protocols provide the ability to instruct staff on appropriate protocols and improves consistency in horse management. Written records provide the ability to evaluate, verify and make adjustments to the biosecurity program over time. Important records include: vaccination, parasite control (deworming), health records, arrivals/departures, contact groups (for example pasture or paddock turnout groups, cleaning and disinfection protocols, protocols for dealing with sick or potentially infectious horses.
Additional resources on diseases and disease transmission:
Section 5: Preventive horse health management program
Goal: There is a horse health management program implemented at the farm or facility that details daily care, disease prevention, and control practices. Every horse on the farm or facility is in compliance with the program to optimize disease prevention in a commingling environment.
Description: Preventive health management programs can improve the health and welfare of horses and increase participation at stables and events by reducing concerns over disease spread. It is important to realize that just as important as your own horses' health is the health of other horses.
5.1 Communication
Goal: The identification or suspicion of horse sickness is promptly communicated to maintain the health and welfare of other horses within a barn or facility where horses are kept. The staff and all the personnel are fully informed of the program and its importance.
Description: Disease notification procedures at farms with a few resident horses and where all owners know each other may be as simple as knowing each other's contact information. At event facilities with large numbers of transient horses that are owned and cared for by various people, communication strategies need to be well planned and documented. A simple, clearly written plan for communicating disease concerns provides a sound foundation for effective management.
Prompt communication of reliable information upon the suspicion or diagnosis of disease is important in:
- consulting with your veterinarian;
- ensuring horse owners, custodians and participants at the farm or facility understand the biosecurity measures being taken and what they need to implement;
- advising neighbouring horse farms and facilities of the disease risk; and
- minimizing anxiety, panic, and overreaction of horse owners and the public.
Figure 7: Example of a simple disease communication and response strategy

Description for flowchart – Figure 7: Example of a simple disease communication and response strategy
There are four arrows in a row each pointing right. There is text written inside and below each arrow. From left to right the text in and below the arrows state:
- Inside the arrow: "When - identification of disease". Below the arrow: "Horse appears to be sick. Establish health criteria that would indicate your horse may be sick - for example a list of clinical signs including changes in behaviour and activity level."
- Inside the arrow: "Who - owner contacts veterinarian". Below the arrow: "Horse owner consults with their veterinarian to determine the cause of sickness and potential treatment and management options."
- Inside the arrow: "What - communication". Below the arrow: "If the disease is easily spread and exposure of other horses is likely to occur, be a good neighbour and let other boarders and neighbours know that your horse is sick."
- Inside the arrow: "How and why - movement controls". Below the arrow: Separate your horse from other horses on the property to the degree possible. Implement movement controls for horses, people, equipment and materials as appropriate to reduce disease and spread."
In situations where multiple horses commingle and many custodians are involved, there needs to be a communication strategy with a designated spokesperson. Inaccurate or inappropriate information may negatively impact the credibility of the farm and facility and the greater horse industry.
It is important that custodians are able to react quickly to minimize the spread of disease to other horses. Owners and operators of farms and facilities where horses commingle (which include events, agricultural fairs, racetracks and auction marts) should have a communication strategy and disease response plan. Participants should be aware of the communication strategy and disease response plan in advance.
Best practices:
Develop a communication strategy tailored to the farm or facility that includes:
- developing a written and signed contractFootnote 7 between the custodian of the farm or facility and the horse owner or specified agentFootnote 8 that requires:
- aligning the preventive care of the horse with the farm or facility requirements;
- sharing all information regarding a health event that could affect other horses on the property;
- pre-arranging a process for disease disclosure to minimize disease spread;
- if your veterinarian is identified as being responsible for disease disclosure, you must provide your veterinarian with written permission to discuss the health concerns of your horse with the owner or operator of the facility;
- identifying an individual to be the point of contact for horse health information from owners and custodians;
- informing the designated individual promptly when a horse is suspected to be sick. If a different custodian provides for the daily care and observation of horse health, give him or her permission to communicate the health concerns;
- identifying a spokesperson in advance who is responsible for sharing information publicly. The spokesperson's knowledge and experience is important for ensuring that the information provided is accurate and presented clearly;
- developing and reviewing the information annually or if any significant changes occur; and
- identifying who is "doing what"; the roles and responsibilities:
- establish and define the biosecurity protocols for the disease situation, how are they different from the routine biosecurity measures and who and how is staff being informed. Ensure the current staff has been trained on the standard operating procedures (SOPs) for managing disease.
Considerations for boarding agreements/contracts and horse health
- A written boarding agreement or contract can improve communication between stable owners and boarders. By clearly outlining roles, responsibilities and expectations, an agreement can provide a predictable outcome when issues arise.
- Provide written permission on who can share information on disease.
- In addition to boarding costs, and services provided, ensure health requirements such as routine vaccinations, parasite control and preventive health care are identified.
- Confirm procedures for communicating medical and non-medical emergencies and providing medical attention for sick, injured or emergency medical situations to ensure the health and welfare of your horse and clarify the financial and legal obligations of both parties.
As provincial acts and regulations differ, research and consult professional advice on when developing boarding agreements/contracts.
5.2 Horse (herd) health management program
Goal: To achieve and maintain a consistent high level of health for all the horses within a farm or facility, develop, implement and maintain a horse health management program.
A preventive health program is only effective if you and other horse owners or custodians comply with the program to establish and maintain horse health. This also applies to horses that are temporarily at the farm or facility including: horses that are visiting, onsite for a short-term event, or only using the facility as a rest stop while in transit.
In facilities where horses are commingled and have been exposed to various environments (for example, shows, events, and other housing facilities) and potential diseases, it is important that the basic health status of the horse be determined and a consistent approach to health management be implemented to ensure the potential risk to resident horses and new arrivals is minimized.
Best practices:
- develop and document the farm or facility health management program in consultation with owners, custodians, veterinarians and other sources of biosecurity expertise (provincial government livestock and extension specialists, industry associations and universities)
- elements of a horse (herd) health program may include:
- premises identification and individual horse identification;
- vaccination requirements prior to entry and protocols post entry;
- disease testing requirements;
- parasite control program (deworming: type of product, timing, testingFootnote 9);
- observation and monitoring procedures for horse health;
- identification of sickness and response procedures; and
- hoof care (including: farrier area scheduling and cleaning; emergency contact info for farrier).
Horse owners and custodians must ensure the horses under their care and the properties they reside on or visit can be distinctly identified to allow appropriate horse health management.
5.3 Monitoring and maintaining animal health
Goal: To promptly identify disease, to minimize potential spread to other horses and to manage the well-being of the sick horse.
Early detection and treatment of sickness provides the best opportunity for a full recovery and reduces the likelihood of disease transmission.
Best practices:
- maintain up-to-date records of management practices (for example, vaccinations and horse arrivals, departures, and contact groups);
- routinely observe and monitor horse health. As a minimum, observation should occur on a daily basis. Increase the frequency of observation and monitoring when horses travel to and return from events, shows, tracks and other activities where commingling occurs (Refer to Annex 4 for information on conducting a horse health check, and Annex 5 and 6 for sample record sheets);
- observation and monitoring of horses includes, but is not limited to, identifying changes in:
- gait and movement;
- appetite;
- manure and urine production;
- mood or disposition and appearance; and
- temperature, pulse and respiration rate.
- establish criteria for identifying a sick horse which would then signal additional action. For example, an increase in temperature above the normal range of 37.0-38.5°C (98.6-101.3°F) should prompt a call to your veterinarian;
- know the normal range for horse vital signs. For an adult horse at rest:
- temperature: 37.0-38.5°C (98.6-101.3°F)Footnote 10;
- heart rate: 28-44 beats per minute;
- respiratory rate: 10-14 breaths per minute.

If there are health concerns, consult a veterinarian. The best practice to minimize suffering of the horse and protect other horses from potential disease, is to ensure there is the capacity for an immediate response.
5.4 Disease response and emergency preparedness protocols
Goal: To protect the health and welfare of horses, develop and implement a disease response and emergency preparedness protocols. All emergency preparedness protocols should include biosecurity considerations. In a disease response, the welfare of the sick horse(s) is protected and measures are implemented to minimize the potential disease risk to other horses. For non-disease emergencies such as flooding and fire, the health and welfare of all the horses are protected during evacuation, transport and housing in an alternative facility.
Description: An immediate response may be required for disease and non-disease related situations. In both circumstances, it is important to have response protocols developed and custodians trained prior to the event. The suspicion or identification of disease at a large facility, particularly a horse show or race track, can result in unnecessary panic, horse movements and other actions that increase disease risks to individual horses and the industry. Events that impact the safety of horses at the facility such as fire, lightning damage and flood may result in the need to evacuate the horses. Evacuation requires pre-planning for transportation and options for alternative facilities.
Best practices:
Animal and premises identification
- ensure all horses at farms and facilities are readily identifiable by all custodians. Post the following information on stables, stalls and paddocks: horse identification (for example, name and accompanying identification including markings, brand, tattoo and microchip ID), charts, and name of owner or individual responsible;
- ensure all premises are distinctly identified; and
- facilitate traceability by permanently identifying horses and maintaining a record of their home premises and owner's contact information.
Roles and responsibilities
- for disease responses and non-disease emergencies, ensure protocols, roles and responsibilities, emergency contact numbers and facility identification (geographic location) are visibly available.
Disease response
Disease response principles for all horse premises and situations are similar; the principles can be applied to one horse in a small farm or facility or for many horses at a large event that are suspected of being sick. The following response can be used for boarding stables or events.
Signs of sickness are identified in a horse - Enhance your biosecurity
- Notify
- Notify the horse owner, or person authorized to act on the owner's behalf, and the farm or facility manager.
- Notify the veterinarian.
- Separate
- Whenever possible, physically separate suspect and sick horses from the other animals and manage them as a distinct group by moving them to a location where contact with other horses cannot occur.
- Depending on the farm or facility size and configuration, this may include housing in a separate stall, a separate barn or pen.
- If physical separation is not possible, restrict access to the horse(s), cordon off an area of the barn or pen to create a temporary separation and indicate that there is a disease concern.
- For both situations wear designated clothing while working with horses, and clean and disinfect footwear, hands and all equipment prior to contact with other horses.
Refer to section 6 for additional details on separation.
- Obtain a diagnosis
- Consult a veterinarian to determine if the horse is infected with a disease that can spread to other horses. If a veterinarian cannot immediately examine the horse, request advice from the veterinarian on measures to prevent further spread.
- The nature of the disease will direct the level of communication and measures of enhanced biosecurity that will be expected to minimize the spread of the disease (Refer to Annex 2 for equine diseases)
- Respond and communicate
- Implement your communication strategy. By sharing accurate information with people directly affected, this will improve disease management and minimize unnecessary overreaction.
- Having your designated spokesperson communicate the information will ensure consistency.
- For large facilities and events, a team of individuals with different backgrounds and expertise is useful for managing the situation.
- Your veterinarian may be required to report certain diseases to the federal or provincial government.
- Identify exposed horses
- Identify other potentially exposed horses - While obtaining a tentative diagnosis, determine which other horses may have been exposed. Focus on those that may have had direct (nose-to-nose) or indirect contact (for example, shared equipment, adjacent stall, shared water, and contact with other participants).
- In general, horses with direct contact are high-risk animals, horses with indirect contact are medium-risk animals, and horses with no known direct or indirect contact can be considered low-risk animals for infection and spread of disease. Knowledge of the disease is important to identify potentially high-risk horses.
- Restrict movement
- Temporarily restrict movements of sick, suspect and exposed horses, along with their handlers, until a veterinarian has made a tentative diagnosis and a response plan is implemented.
- In many situations, a veterinarian will be able to narrow down the possible cause of the disease by obtaining a thorough history, a review of associated horse health records, and a physical exam of the horse.
- Depending on the circumstances, low- and medium-risk horses can continue to compete; however, minimize direct and indirect exposure.
- Restrict movement of other animals on the farm or facility.
- Monitor horses
- Observe sick and exposed horses for changes in health status as per veterinary instruction. Twice daily observation and monitoring of rectal temperatures is a good practice for all horses attending the event.
- Release horses
- Prior to removing movement restrictions, consult with the attending veterinarian.
- Brief all participants leaving the facility or event about the disease and the need to monitor their horses for sickness.
- Horses that are sick and/or exposed through direct and indirect contact should upon their return home, be separated from other horses and monitored, and treated as appropriate until their sickness clears or their health status is determined.
- Unexposed horses may be transported to other venues. It is a good practice to disclose your previous attendance at an event where an infectious disease was present.
Non-disease response - Emergency preparedness action plan (for example, flood, fire, natural disaster)
Develop an evacuation, transport and alternative facilities plan to protect the health and welfare of horses while considering biosecurity continuity. The evacuation protocols should minimize chaos and optimize the timely removal of horses in a systematic process that includes continuity of identity. Establish and pre-arrange an emergency transport plan and housing in an alternative facility for short- and longer-term emergencies;

Emergency personnel responding to a fire at a horse barn in Ontario. Photo courtesy of Gary Dinkel - Recognize that horse behaviour, particularly when frightened by the threat of fire or other disaster, can be unpredictable. Practice evacuation plans to increase the opportunity for success;
- Ensure there are sufficient halters and lead ropes stored in a location away from the barn that are easily accessible;
- Designate custodians to specific tasks. For example, a person designated to manage transportation, manage the systematic removal of horses and ensure identification is available for each horse during transport and subsequent placement at the alternative facilities; and
- The preservation of life is the primary objective. Once the threat has been mitigated, if biosecurity protocols have been compromised, then perform a situation assessment and implement appropriate biosecurity measures.
Section 6: New horses, returning horses, visiting horses, movements and transportation
Goal: Movement of horses is done in a manner that minimizes the risk of introduction and spread of pathogens.
Description: New horses may pose a significant risk for introducing disease to resident horses. It is important to determine the health of new horse(s) and ensure you have sufficient space and people to perform routine care prior to adding them to your herd.
6.1 New horses (purchase consideration), new arrivals, and returning horses
Goal: Determine the health status of new horses and align the health status with the resident herd. This will direct the procedures that may need to be taken before introducing horses to the herd. Separate and implement measures for newly arriving and returning horses to protect the health of other horses.
Description: New horses may bring disease to your herd. While it is easy to identify visibly sick horses and separate them from other horses to reduce disease spread, the sub-clinically infected horses (they appear healthy, yet carry a pathogen) pose a challenge. This is why routine measures to Separate All Incoming horses from resident horses are important. Although measures can be taken to reduce this risk (for example, testing for diseases and veterinary health exams prior to arrival), some infected horses will not be identified through these methods, depending on the tests used and the stage of infection.
Returning horses may also pose a risk for introducing disease depending on their potential exposure while off the farm or facility. Be sure to consider the length of time your horse has been away and the risks associated with the activities and locations of your horse(s) prior to, and on return to, the farm or facility of origin.
Separating all incoming horses for a period of time is a good strategy for reducing the risk of introducing disease to resident animals
Best practices:
- prior to new horses arriving, obtain proof (documentation) of the vaccination, deworming history and other health tests as required (for example a recentFootnote 11 negative test for equine infectious anemia {swamp fever} and other diseases). When this is not feasible, perform these tests while the horses remain separated from other horses (Refer to Annex 9 for a sample Incoming Horse Protocol Record);
At large events, require official documentation of health status (certified by a veterinarian)

Description for image – A biosecurity sign
The biosecurity sign contains text that states: "WHOA. This Facility requires a negative Coggins (EIA) test prior to off loading or entering the premises with your Horses. Contact Area Management." There are spaces provided to write the contact information of the area management. At the top of the sign there is a red hexagon on either side of the word WHOA. Each hexagon has text inside it written in white letters that states "STOP".
This large sign makes it clear that a negative Coggins test for EIA is required for entry to the premises. Having contact information for the arena manager is a good practice for addressing issues. For privacy reasons, the phone number has been removed from this photo. Photo courtesy of Alex McIsaac DVM

Description for image – A square, white biosecurity sign
A square, white biosecurity sign. The border of the sign is outlined with a solid red line. In the middle of the sign is a red square. There is text inside the red square that states: ATTENTION in white, capital letters. Above the word attention and overlapping with the red square is a drawing of a person riding a horse. The drawing is solid black. There is text written above the drawing that states: "Cambridge Meadows Equestrian Centre". Below the red square there is text that states: "Preventing the spread of disease is important to Cambridge Meadows. Only healthy horses allowed entry to grounds. Only clean equipment and tack allowed on-site. On arrival all participants must present health certification to event officials. A negative EIA test within the last 6 months is required. Horses must be presented on entry for a health check. Participants to report signs of horse sickness to event officials immediately. Failure to adhere to these requirements may result in disqualification."
This facility leaves little doubt as to their commitment to managing horse health. They have identified the disease risks posed by equipment and tack and the need to report sick horses to event officials.
The sign is a good reminder to participants of their responsibility for establishing the health of their horses and the consequences for failing to comply may result in their disqualification. Ensuring boarders and participants/visitors are aware of the requirements helps to protect the health of all horses.
Ideally, the requirements are provided to horse owners and custodians prior to the event and again on arrival at the facility.
Image courtesy of Daniel Schwartz DVM
- review the health records detailing past sickness, treatments, veterinary exams and travel history when available;
- ensure horses are distinctly identified: records of distinct and unique markings can be helpful;
- when purchasing multiple horses, purchase from as few sources as possible to minimize exposure to disease. When this is not feasible, as at yearling sales, more emphasis will need to be placed on biosecurity during transport and at the home location;
- when purchasing multiple horses, consider managing them as groups based on similar risks. Possible groupings might include previous ownership, health status, age, and type of use;
- if using semen and embryos, ensure donor animals are free of venereal disease and acceptable veterinary methods were used for collection, processing and storage of semen and embryos;
- separate new arrivals from the resident horses on the farm for a period of time sufficient to give you confidence that they are free from disease. There are a number of factors that influence the length of the separation period. Consult your veterinarian to identify an appropriate time;
- The separation period normally recommended exceeds (is longer than) the time frame for clinical signs to develop following exposure to the diseases of concern. Health management practices including vaccination and deworming protocols and the travel history of new horses are important in determining potential diseases risks. Proof of vaccination and negative test results should be obtained;
Some suggested time frames for separation are:
- 5 to 7 days for horses of known high health status, which includes no known recent contact with sick horses, a thorough medical history and a recent veterinary exam with negative results;
- 14 days for horses of a similar health status and from a similar facility or farm health management program;
- 21 to 28 days for horses with undetermined health status or arriving from facilities where the horse health management program is unknown or components of the health program are absent.
You may be able to shorten the period of separation if you obtain:
- negative test results for key diseases;
- a thorough medical history; and
- a recent veterinary health exam with negative results.
- ensure farm or facility managers obtain a certificate of veterinary examination completed within 7 days prior to entry to determine the health status of the horse and the biosecurity procedures that are appropriate (for example, vaccination and disease testing where possible; this may not be feasible at a sales auction);
- vaccination: (Refer to Annex 10 for additional guidance on vaccination)
- assess the vaccination needs of your horse(s) with your veterinarian. Some factors to consider are the: horse's age, vaccination history, exposure to and prevalence of disease in their environment and their travel history.
- note: vaccination does not provide immediate protection from disease and many vaccines require two or more doses over a period of three to four weeks. Horses that have not been properly vaccinated against a specific pathogen can be vaccinated prior to entry to the farm or facility. When this is not feasible, these procedures may also be performed while horses are separated on the farm or facility;
- vaccines should be administered according to the label instructions;
- only obtain vaccines from reputable sources to ensure they have been handled and stored appropriately;
- keep records of vaccination (date administered, vaccine type and manufacturer's specific identification such as lot number); and
- report any adverse effects that occur to your veterinarian and the manufacturer of the vaccine.
- assess the vaccination needs of your horse(s) with your veterinarian. Some factors to consider are the: horse's age, vaccination history, exposure to and prevalence of disease in their environment and their travel history.
Some provinces regulate and restrict who can administer vaccines. Ensure you are aware of and comply with the regulatory requirements.
Vaccines are best administered by your veterinarian who has knowledge of their benefits, risks and appropriate use to protect the health of your horse(s).
- manure testing of new horses should be done using fecal egg counts to determine the horse's worm burden prior to deworming and enrolling in the farm's parasite control program;

- fecal egg count reduction (FECR) testing should be considered to evaluate response to deworming and detect any resistance of the parasites to the dewormer; (Refer to Annex 11 for additional guidance on parasite control)
- physically separate horses to prevent direct or indirect contact between the new animals and resident horses. When physical separation is not possible, procedural barriers can be used. This involves limiting the number of people who enter the horse's stall to dedicated staff only, the use of gloves or hand hygiene (hand washing), clean or dedicated clothing for those handling the horse, and preventing nose to nose contact with neighbouring horses. Keep in mind that procedural barriers do not decrease the risk of disease spread to the extent of physical separation. Similarly, physical barriers are insufficient to prevent disease if procedures to minimize cross contamination are not applied. When using either physical separation or procedural barriers, dedicate equipment or clean and disinfect equipment for these horses. Restrict access and control the movements in the area where the new horses are located;
- monitor new horses daily for any change in their health including daily body temperature assessments and record these findings in a log book; and
- immediately separate and have a veterinarian examine any horse suspected of having a contagious disease such as diarrhea, respiratory disease or a fever of unknown origin (Refer to Annex 13 for additional guidance on separating sick horses).
Important considerations:
- Crowding and the stress of transport and unfamiliar herd mates can reduce a horse's resistance to disease and result in the shedding of pathogens.
- Breeding centers can pose a risk to the health of stallions, mares, semen, and embryos through horse-to-horse contact during live cover breeding and from contaminated equipment. Appropriate hygiene is necessary to minimize transmission of pathogens during these processes and contamination following the collection and storage of embryos and semen.
- Horse sales and auction barns can pose significant risks to horse health where there is the opportunity for commingling, the shared use of halters, lead ropes, water troughs and stalls. Additionally, be aware of the historical health status of the facility (for example, endemic strangles).
6.2 Visiting horses
Goal: Decrease the risk of disease transmission from horses visiting the farm or facility for a short period of time (for example, lessons, training, day events, recreational riding and breeding).
Description: Visiting horses that do not share the same health status of the resident herd may pose similar risks as new arrivals to a farm or facility if permitted to commingle. Visiting horses that will be housed on the farm or facility require the same biosecurity considerations as new horses.
Best practices:
- the health status of the visiting horses should be determined before they arrive, and should be consistent with the health management program at the farm or facility;
- equipment accompanying visiting horses should be clean and used only for those horses (for example, trailer, tack, grooming equipment, feed and water buckets). This may include the following: ensuring that the trailer has not been exposed to a horse that has a disease (clean and disinfect when appropriate i.e. a borrowed trailer) parking in a designated area, bringing clean and disinfected buckets to water and feed visiting horses (Refer to section 8.5 and Annex 15 for additional information on cleaning and disinfection), and not permitting commingling;
- ensure paddock and stall areas are available that allow for separation of the visiting horse(s) from the resident herd;
- do not allow horses to have direct contact during activities; and
- at facilities that have all or a large percentage of the population coming and going such as with racehorses at training facilities, separating horses may not be practical or accommodated with the facility design. In these situations, separate the resident horses that never leave the premises (for example, teaching or retired horses) or young horses such as yearlings or breeding mares from those coming and going. Racing horses should be kept together in adjacent stalls and separate from yearlings and two-year-old horses in training.
6.3 Movement within the farm or facility
Goal: Horse movements within a farm or facility are managed to reduce exposure from higher-risk horsesFootnote 12 to horses with lower disease resistanceFootnote 13.
Best practices:
- house horses of similar risk groups (health status, use, and age) together and limit cross-contact between personnel, equipment and exposure to common environments (paddocks, pastures);
- house mares and foals separately from the remainder of the herd; and
- maintain the physical separationFootnote 14 of sick, new, returning, and visiting horses from the resident herd.
Horses that play together should stay together.
6.4 Attendance at events
Goal: Minimize risks for disease transmission from horses and equipment (buckets and tack) taken to and returning from events.
Description: Commingling of horses at events pose a significant risk for disease transmission. Participants and event organizers share responsibility in minimizing these risks and have complementary roles.
6.4.1 Responsibility of the custodian
Best practices:
- review health requirements (for example, is a negative EIA test required?);
- ensure horses are healthy and properly vaccinated. Consult your veterinarian regarding timing of vaccinations;
- manage horses from the same barn or farm as a group and stall together at the event;
- minimize contact between riders, grooms, trainers and coaches with horses that are not their own;
- dedicate equipment to your horses and prevent sharing amongst horses. This includes, but is not limited to, blankets, feed tubs, water buckets, tack, grooming supplies, and stall cleaning equipment (Note: riders' pant legs and footwear should be cleaned prior to switching horses)
- visibly identify equipment to prevent sharing;
- ensure supplies, such as hand sanitizer, soap, brushes and disinfectant for cleaning and disinfection are provided or brought to the event and the assigned stalls cleaned if necessary;
- check with the event organizer or racetrack to determine what methods are used to clean and disinfect the stall or paddock area between use by different horses (refer to Section 8.5 Annex 15 for additional information on cleaning and disinfection);
- monitor your horse's health including body temperature daily while at the event. Report any abnormalities to the event organizer (and veterinarian; event designated or other). Keep the event organizer informed of any changes to the horse's condition;
- avoid any form of direct (for example, nose-to-nose) and indirect (for example, common surfaces in wash stalls) contact between horses;
- consider using your own water hose; and
- do not submerge the end of a common use water hose into a water bucket.
6.4.2 Responsibility of the event organizer
Best practices:
- it is the responsibility of the event organizer to establish health requirements for entry (for example, risk-based testing may be required prior to entry to the grounds [e.g., EIA, strangles and EHV-1]);
- restrict spectator access to the stabling area or to the trailer area;
- ensure stall areas have complete barriers between horses;
- provide specified stalls and areas for sick or suspect horses;
- ensure stalls are cleaned and disinfected prior to arrival and between each horse (post a visible record of cleaning);
- ensure wash stalls are cleaned and disinfected frequently and ideally, between horses (post a visible record of cleaning);
- provide approved sharps containers in adequate numbers;
- provide hand sanitizers or hand wash stations in the stabling area;
- establish veterinary services for the event (for example, on-call or on-site);
- recommend that horse custodians take and record resting horse temperatures at least once per day and the record be made available for verification by event officials; and
- ensure all equipment used at or brought to an event is cleaned and disinfected (for example jumps, portable stalls).
(Refer to Annex 7 for a sample horse participant declaration and Annex 8 for a sample event letter to horse participants)
An industry best practice is to have the person with legal authority for the care of the horse sign an agreement that requires informing the event organizer of a health issue that is potentially infectious. The event organizer, with veterinary guidance, will implement the biosecurity protocol that has been developed.

Tips for trail riders:
- When trail riding with friends or neighbours, it is good practice to know the health status and history of the other horses beforehand. This may be as simple as ensuring horses are of the same health status and have no signs of sickness prior to gathering.
- Avoiding nose-to-nose contact with other horses and maintaining a distance of 2 m from other horses while on the trail can reduce opportunities for disease spread.
- Avoid sharing tack, equipment, water buckets and feed.
- Manage what your horse eats - Prevent them from consuming feed or water supplied to other horses.
- If staying overnight along the trail or in a campground, ensure all previous feed, bedding and manure from the horse stabling area is removed prior to unloading or bedding down your horse.
- Wipe down common contact surfaces such as hitching rails and tie lines, and leave space between horses.
- Remove and dispose of feed, water and bedding from the camp location on departure so it is clean for the next rider.
References Footnote 15 Footnote 16
6.5 Transportation
Goal: Horses are transported in a way to minimize exposure to or spread of disease.
Best practices:
- ensure horse transport complies with all applicable legislation including the requirements in the Health of Animals ActFootnote 17 and RegulationsFootnote 18 and the Code of Practice for the Care and Handling of EquinesFootnote 19;
- transport only your horses or at least only those for which you know the management and health status;
- a horse that shows signs of or is compromised by infectious disease should only be transported to a facility where it will receive proper care and should not be transported with healthy horses (clean and disinfect the trailer before it leaves the care facility);
- minimize social stress when transporting horses on the same trailer;
- avoid mixing young horses when shipping (for example, yearlings mixed together from different farms or with young racehorses);
- tie your horse to your own trailer to minimize exposure to pathogens from other trailers; and
- after transporting horses, clean to remove all organic material and disinfect the trailer.
Section 7: Access management
Goal: Management and control of farm or facility access and identified risk areas limit disease introduction and spread on-site and enable the implementation of biosecurity practices.
Description: Access management refers to the use of physical barriers and/or procedural measures to reduce the transmission of pathogens onto, within and between horse farms and facilities by people, horses, equipment, materials, vehicles and trailers.
Essentials of access management include:
- Identifying pathways for disease transmission;
- Interrupting or blocking pathways of disease transmission;
- Controlling unwanted or unnecessary access to a farm, facility and horses;
- Managing the movement of people, horses and equipment on site; and
- Employing biosecurity measures to reduce the risk of exposure to and spread of disease should an outbreak occur.
Consideration given to proper access management in the early implementation of biosecurity plans provides an improved capability to respond should disease occur.
7.1 Movement onto and within farms and facilities (zones)
Goal: Establish and identify biosecure zones, controlled access points, and pathways to control access to the premises, barns and horses and to minimize pathogen transmission by animals, people, vehicles, trailers and equipment.
Description: Biosecure zones simply allow the separation and protection of horses and areas used for their care from sources of pathogens by mapping out and then controlling movements of people, animals, equipment and materials through zones. It starts with dividing a facility into management areas and identifying access points (controlled access points) to each area. Management areas might include the site as a whole, an individual barn, or arenas and other locations, including wash stalls and feed rooms. Controlled access points should be equipped with the necessary materials and supplies to implement biosecurity procedures.
The design of zones and applicable biosecurity requirements should reflect the specific disease risks and the management goals of the equine owner, custodian or facility manager. Properly established biosecurity zones facilitate day-to-day activities without the unnecessary interruption associated with application of dissimilar biosecurity procedures. In many countries, including Canada, zones for controlling movement and biosecurity management, are called either controlled access zones or restricted access zones based on the risk of activities carried out within them.
- A controlled access zone is a designated area that contains the land, buildings, equipment and infrastructure involved in the care and management of horses where access and movements are controlled. Entry is restricted and managed through a controlled access point. The controlled access zone is often the first zone that is entered on a farm or facility and frequently includes laneways, equipment, storage sheds, and riding arenas, although some of these may be in the restricted access zone in other facilities. It usually excludes the house and office space of the farm owner and manager. The controlled access zone may include pastures and barns that horses are not currently occupying. A controlled access zone has its own specific biosecurity protocol and often encompasses the restricted access zone(s).
- A restricted access zone is a designated area where horses commonly reside (are stabled, housed, pastured) and where access to people, equipment and materials is further restricted. The zone(s) include the pens, barns, and pastures, as well as separation areas used for new, visiting and sick horses. The layout and management practices of individual farms and facilities will determine whether manure storage and other production infrastructure directly involved in animal care and maintenance should be included within the restricted access zone.
It is important to remember that equine owners and custodians may decide to use a single zone to manage biosecurity on a farm or facility, depending on its complexity and risk factors that exist.
Figure 8: Zoning on a horse facility:

Description for image – Figure 8: Zoning on a horse facility
A picture of a horse facility surrounded by a fence painted yellow. Outside the fenced area in the bottom right is a house. To the left of the house is a parking area (concrete pad) with a number of horse trailers and pick-up trucks parked on it. Between the parking area and the horse barns and grounds is a large closed gate. In the lower left of the picture are two biosecurity signs. One is a large rectangular white sign with the text "Visitors please respect farm biosecurity. Phone or visit the house before entering. Do not enter property without prior approval. Keep to laneways and pathways." A smaller yellow sign in the shape of a yield sign has the text: "Biosecurity in effect. Do not enter." Behind the gate starting from the left side is a horse pasture surrounded by a white wood fence with a gate. There are a number of horses in the pasture and a large water trough. To the right is a horse arena surrounded by a fence, a gate and some bleacher seats. Behind the arena is a covered manure storage area on a concrete pad. To the right of the arena is a large horse barn with the barn doors open at the front. To the right of the barn are fenced turnout pens. A storage barn is located below the turnout pens. Hard surfaces surround the horse pasture, barn and storage barn.
A simple horse facility demonstrating the concept of two biosecurity zones. The controlled access zone (yellow fenced area) establishes a boundary between everything outside the facility and areas of the property involved in horse care and management. It provides the ability to manage the risks of the introduction of disease into areas where it may be easily transferred to horses and reduce the spread of disease off of the property. Storage areas for feed, bedding and manure and bleachers for viewing the arena are located in this zone. Restricted access zones (areas bounded in red) require stricter biosecurity and limit direct access to horses or the areas that they may reside. Controlled access points (purple gates) and signage assist in managing and directing traffic flow into and out of the controlled and restricted access zones. Parking for visitors is established outside the controlled access zone and a separate driveway and parking area is established for the property owner's house.
Figure 9: Zoning on a horse facility

Description for image – Figure 9: Zoning on a horse facility
A picture of a horse facility surrounded by a fence painted yellow. Outside the fenced area in the bottom right is a house. To the left of the house is a parking area (concrete pad) with a number of horse trailers and pick-up trucks parked on it. Between the parking area and the horse barns and grounds is a large closed gate. Behind the gate starting from the left side is a horse pasture surrounded by a white wood fence with a gate. To the right is a horse arena surrounded by a fence, a gate and some bleacher seats. Behind the arena is a covered manure storage area on a concrete pad. To the right of the arena is a large horse barn with the barn doors open at the front. To the right of the barn are two fenced turnout pens and at the top back right corner a fenced turnout area with a small horse shelter. A storage barn is located below the turnout pens. Hard surfaces surround the horse pasture, barn and storage barn.
An alternate view of the horse facility depicted in figure 8. Clockwise from the upper left: Pastured horses are separated from other horses on the property and traffic flow minimizes interaction with resident horses. Covered manure storage is located at the back edge of the property with a dedicated controlled access point (purple gate) allowing access and manure removal, minimizing entry into the property. The arena and resident horse barns are restricted access zones. Hard-surface pathways facilitate movement around the property and completely surround the barn, which is a high traffic area.
In the upper right-hand corner, a restricted access zone surrounds a small barn (stable) and paddock area established for the care of sick or suspect horses. Separate feed, water, equipment and tack are stored here and dedicated for the care and maintenance of horses. Two day turn-out paddocks (also restricted access zones) allow separation of peer group horses. Feed and bedding are stored in the small barn adjacent to them.
Best practices:
- review farm or facility layout to determine what biosecurity risks exist with current horse stabling locations;
- establish controlled access zones and restricted access zones and, when necessary, establish segregation areas for new horses, for horses returning from off farm events, and areas for the treatment of sick horses;
- minimize unnecessary access by limiting the number of entrances (access points);
- ensure the necessary biosecurity equipment is provided at designated access points;
- establish and identify pathways to reduce the risk of disease spread by separating the movement of horses of different health status, used and new materials (bedding), visitors and farm personnel;
- maintain the pathways clean and free of potential sources of disease; and
- post biosecurity signage to guide and direct custodians and visitors.
Best practices: Large event facilities
- apply farm or facility zoning "best practices" to the degree possible;
- manage the access and movements of people and pets on-site;
- establish separate entrances and parking areas for participants and visitors;
- ensure resident horses, if present, are housed and exercised separately from visiting participant horses. If this is not possible, ensure resident horses are required to be held to the same health status as competition horses;
- encourage the use of housing that prevents nose-to-nose (direct) contact between horses;
- ensure common use areas such as wash stalls or racks prevent direct contact between horses and to the degree possible, common contact surfaces (fomites);
- stable horses in groups (cohorts) to create distinct management units with their own wash stalls, feed and equipment storage; and
- establish a segregation area for sick horses that is physically separated from the housing and exercise areas used by resident and participant horses.
7.2 Procedures for moving between zones
Goal: Establish requirements and implement procedures to manage the entry and movement of people, horses, equipment, vehicles and trailers.
Description: To achieve the benefits zones can provide depends on controlling access to the zone(s) and the application of appropriate biosecurity measures when people, horses, equipment, vehicles and trailers cross zone boundaries.
People, particularly those who have had contact with livestock or other livestock premises, and horses, primarily those that are of an unknown or lower health status, that enter the farm or facility pose a risk for the introduction of disease. Additionally, pathogens that may be present in manure, respiratory fluids, urine and blood, can contaminate equipment and trailers and transmit disease when they come into contact with horses.
The biosecurity measures required for people, equipment and horses moving across zones can be viewed as a gradient occurring at different levels based on risk. As the risk of the introduction and transmission of pathogens increases, the degree of biosecurity measures required increases.
Veterinarians can assist equine owners and custodians in assessing what risk factors exist with a particular event or facility, and how to institute practices consistent with the risk at hand.
In some facilities, biosecurity levels are identified by colour (for example, green, yellow, red). Colour-coded biosecurity signs indicate the level of biosecurity and biosecurity practices to be followed.
Basic biosecurity practices include those conducted on a daily basis as a part of normal care and husbandry. Biosecurity protocols at a basic level describe routine practices for things like personal sanitation, (for example hand washing), handling of animal waste, use of water hoses and buckets, handling feed, care and sanitation of tack and grooming supplies, and routine monitoring of health.
As the level of precaution increases, basic biosecurity practices still apply supplemented by protocols limiting access; describing the care and use of protective clothing for certain areas; stricter levels of personal sanitation between every horse, greater level of control over the hygiene of tack, grooming supplies, water pails and feed tubs, including restrictions on sharing between horses. Direct nose-to-nose contact between horses over stalls and fences would be controlled.
At an enhanced level of biosecurity, access to certain areas is restricted and controlleddue to disease, or the need for separation for any reason (for example, post-import separation). Biosecurity protocols for restricted areas include all measures mentioned above plus expanded attention to posted signs and instructions. Sanitary precautions are carefully outlined including the cleaning and disinfection of footwear and use of disinfectant footbaths.
Larger boarding stables and event venues pose an increased risk for disease transmission due to:
- increased numbers of horses;
- potential for uncontrolled commingling of horses with different health management backgrounds; and
- more frequent movement of people, horses and equipment and the associated stress of transport.
Day-to-day access management in large facilities is more difficult to accomplish, increasing the importance of vaccination programs, prescribed health standards for attendance, and monitoring the health of horses in attendance.

Best practices - People:
- train personnel on-farm and facility biosecurity procedures;
- limit non-essential traffic on the site and restrict unnecessary access to horses;
- prevent visitor access if they have had recent contact (< 48 hours) with horses suspected or known to be infected with a contagious disease;
- prevent visitor access if they have recently returned (< 5 days) from a foreign country where contact with horses or livestock has occurred;
- restrict access to horses separated from the resident herd (those that are sick and new or recently returned horses) to only those personnel necessary for their care;
- plan ahead for visitors by informing them of the farm/facility biosecurity procedures in advance of their arrival;
- schedule visitor arrivals, particularly visitors with horses of unknown health status;
- meet new and infrequent visitors at the farm/facility entrance (outside the CAZ) and provide biosecurity instructions. For frequent visitors, consider reviewing biosecurity procedures with them, e.g. twice a year, and randomly checking their compliance to procedures;
- use a visitor log to document visitor access which will assist with disease control and response activities within the industry;
- provide a means for participants to report biosecurity concerns to facility managers for action
- assign staff to monitor movements within the venue including access to barns, isolation areas and to provide guidance to participants and visitors on which areas of the venue they are allowed to access;
- restrict access to the isolation area to only those people necessary for the horses' direct care; and
- restrict access to horse management units to only those horses and participants assigned to them.
Best practices - Sanitation (people, equipment, tack)
- hand washing or the use of a hand sanitizer, combined with barrier protection (protective outer clothing or clothing changes) are effective measures for reducing disease transmission by people;
- dedicate equipment and tack to each horse (halter, lead rope, brushes, rags, water and feed buckets, hay nets, fly masks etc.);
- clearly identify dedicated equipment by labelling or colour-coding;
- clean and disinfect shared equipment between horses;
- clean and disinfect equipment at the end of the day and store in a clean location separate from other horse equipment;
- select equipment that can be easily cleaned and disinfected, where feasible: hard and non-porous surfaces (metal, fiberglass, plastic, rubber) rather than softer porous materials (wood or easily scratched synthetic material);
- dedicate equipment to areas where horses are separated from the herd while sick or for a period of observation;
- only allow equipment, tools, and vehicles that have been brought onto the site to enter a control area if it is necessary;
- ensure visitor vehicles are visibly clean prior to entry to the premises and control access zone. Can request additional measures if the vehicle is coming from an area where disease has been present;
- ensure service equipment (farrier etc.), tools and vehicles have been cleaned and disinfected prior to entry; and
- follow a stepwise procedure for cleaning and disinfection and use a registered disinfectant (Drug Identification Number) that targets the pathogens of concern.
Section 8: Farm and facility management
Goal: Promote horse health by providing a clean, well-maintained, low stress, and safe environment that minimizes biosecurity risks.
Description:
Farm and facility management includes, but is not limited to, any structures that may house or shelter horses, paddocks, pastures, equipment, bedding, feed and manure storage areas, as well as riding arenas, race tracks and show areas. The implementation of proactive biosecurity in all aspects of the farm and facility management is important to the health and well-being of horses.
8.1 Feed, water, and bedding
Goal: Obtain good quality feed, water, and bedding and protect them from contamination by manure, water, pests, and wildlife.
Description: Good quality feed, water, and bedding are vital to horse health. The source, processing, transport and storage of feed, water and bedding are important considerations to minimize exposure to pathogens.
Best practices:
Feed: The main cause of sickness from feed is not transmission of infectious disease but moulds causing digestive problems and toxemia; these are not spread from horse to horse. However, feed can become contaminated by other pathogens and cause sickness in horses.
- for optimum health, determine and discuss the nutritional (feed) requirements for your horse(s) with a horse nutritionist or your veterinarian;
- obtain and provide high quality feed from a known source, either a commercial feed mill with a quality assurance program or from a supplier that has protocols to ensure raw materials are harvested, stored, and transported to lessen the chance of contamination;
- collect and store a representative sample of each feed shipment for testing and analysis;
- store concentrates and roughage in a manner that prevents contamination (by water, pests, wildlife, urine and manure) or spoilage. Storing feed in a separate building from the horses can minimize rodent activity in and around horses;
- dispose of feed that is contaminated or substandard quality;
- use feed in a manner which rotates oldest to newest; and
- entirely empty your feed storage containers between each batch.
WaterFootnote 20: While there are a few options for sourcing water (private well, public water supply, rivers, lakes and ponds), some are more variable in their quality and may pose a risk of disease to your animals. Water should be tested annually and where necessary (for example, change in water colour or odour). Treatment of water (for example, UV filtration) may be required to ensure quality and minimize the risk of contamination.
Water quality and palatability are affected by temperature, pH salinity, pathogens (for example, coliforms and blue green algae), minerals, and chemicals. Surface water sources (for example, ponds and creeks) have more variability in quality and increased opportunity for contamination than wells and public/municipal water supplies. Diseases such as leptospirosis, giardiasis, equine protozoal myeloencephalitis (EPM) and botulism may be a higher risk when using surface water sources.
The benefits of public water suppliers are that they are responsible for ensuring the quality of commercial water. Although of less concern than shallow wells, ponds and streams, it is important to recognize publicly supplied water may be contaminated. Contamination may occur by inappropriate treatment, poorly maintained distribution system to the facility, or poorly maintained water distribution system at the facility. Routinely clean, disinfect and flush the water distribution system. This includes buckets, troughs and automatic waterer systems.
Note: The use and access of surface water sources by livestock is often regulated by acts and regulations to protect ground and surface water quality and environmental habitat. Horse owners and custodians are reminded to ensure compliance with the relevant legislation.
- communal (shared) water sources can be a source of transmission of pathogens. Where horses are comingling at a temporary location (event, show), provide water to all horses individually, preventing the sharing of water buckets or the use of common water troughs;
- identify the source of the water and evaluate for quality and palatability;
- do not submerge common use water hoses into water buckets;
- where possible, prevent access to natural surface water sources; and
- test water quality at least annually to ensure it meets standards for livestock consumption.Footnote 21 Consider testing surface water sources and shallow wells:
- following periods of heavy rain and runoff if there are concerns over contamination from manure or other contaminants;
- if there is a change in the taste, colour or odour of the water; and
- if there is widespread unexplained sickness in the herd.
Ideally, horses should have their own water buckets; they should not be shared between risk and peer groups (for example, new horses and horses with suspected sickness).
Bedding: Used bedding and new bedding (if not properly sourced, transported and stored) can be a source of pathogens.
- store fresh bedding in a manner that prevents contamination by manure, water, pests and wildlife;
- provide a consistent source of dry absorbable bedding which is removed and replaced when soiled and on a regular schedule with a stall cleaning routine;
- remove bedding and clean and disinfect stalls prior to placing a different horse in the stall. It is particularly important to ensure that the stall has been disinfected if it was occupied by a sick horse; and
- ensure the disinfectant selected and protocol used is appropriate based on the type of walls and flooring (for example, wood, concrete). Refer to Annex 14 for additional information on Disinfectants and Annex 15 for additional information on cleaning and disinfection procedures.
8.2 Property and pest management
Goal: Maintain the property to provide a healthy and safe environment for horses. Minimize pest and parasite populations; manage pet activities, and exposure to wildlife through an integrated pest management and wildlife control plan.
Description: Properly storing equipment, feed and manure, as well as keeping the facility and surrounding area free of debris is important for the health and safety of horses. Unobstructed areas allow for cleaning and minimize the potential risk of injury to horses. It is also an important element of pest and wildlife control.
Pests and wildlife are opportunistic. Discarded waste, spilled feed or objects present opportunities for a meal or establishing a home. Pests, domestic pets, feral animals, livestock, parasites, and wildlife can cause or transmit disease and cause physical irritation and injury to horses. Insects (particularly flies, mosquitoes and gnats) and rodents are the most common pests that must be managed. It is important to initiate primary methods of pest and wildlife control by reducing sources of habitat and attractants prior to initiating secondary measures such as insecticides and pesticides.
Best practices:
- initiate primary methods of pest control by reducing sources and habitat for insects and pests;
- keep vegetation mowed short;
- compost or contain manure;
- remove hiding and nesting areas for pests and wildlife;
- minimize pooling water on the site by grading, adding fill and controlling water runoff; and
- eliminate other insect breeding sites by removing objects such as tires, buckets, pots and debris where stagnant water can accumulate, keep roof gutters and water catchment free of debris.
- install fans in barns to reduce moisture in barns and bedding where insects can breed and to limit entry of flying insects;

- feed is an attractant for pets, pests, wildlife and other domestic animals. Securely store feed, promptly clean up feed spills and properly store garbage;
- as necessary, treat horses and/or the premises with repellents and insecticides on a seasonal basis and according to manufacturer's recommendations. Consult a pest specialist (exterminator) if required when managing significant infestations;
- use a variety of fly and insect traps to help manage populations around barns and pastures;





- install live traps for rodents and monitor their activity. Use rodent bait stations and traps only after careful consideration and with caution as they pose a threat to pets, wildlife and children;
- screen windows and doors and seal openings to barns and facilities;
- move horses inside during high risk times (for example, dusk to dawn) during the vector season;
- minimize contacts with pets, other livestock and wildlife, which can act as potential disease vectors; and
- keep horses away from farm equipment storage areas.
Additional information on pest management:
Mosquito and Fly Prevention and Control on Manitoba Farms: Manitoba Agriculture, Food and Rural Initiatives, Soils and Crops Branch
Insect Pests: Penn State Extension
Fly Control Around Horses: University of Minnesota Extension
| Method | Comments |
|---|---|
| Natural method Bats and birds |
While bats and some bird species (swallows and purple martins) consume large volumes of insects, there is insufficient scientific evidence to support encouraging their presence around horse properties to control flies, mosquitoes and gnats. |
| Natural method Parasitic wasps (Muscidifurax raptor, Muscidifurax raptorellus & Muscidifurax zaraptor) |
Small, nocturnal, non-stinging wasps that lay eggs in fly pupae. The developing wasps kill the fly pupae. Wasps need to be released early in the spring and every 2 to 4 weeks until frost. Targeting pupae rather than adult flies can significantly reduce fly populations by decreasing opportunities by adult flies to lay eggs. Can be used to control many species of flies. Wasps (parasitized fly pupae in shavings) can be purchased and shipped from Canadian companies. |
| Traps | A variety of traps target adult flies, some of which have fly attractants or baits. Some options include sticky fly tape, baited containers, and horse fly traps. Fly traps are often only effective against certain species of flies so different types of traps need to be used. Traps need to be properly placed, monitored and replaced frequently. |
| Repellents | Many formulations and products are available; meant to repel rather than kill insects. Products are variable in their effectiveness and duration of action.
|
| Insecticides | Chemicals that primarily target and kill adult flies. Products that are formulated for external application include (among others) sprays, pour-on, spot-on, wipes, and powders. Some products can be used as environmental sprays/barn sprays: Common ingredients include:
Insecticides are regulated by the Pest Management Regulatory Agency of Health Canada. To be registered, products must be proven to be effective, and pose minimal risk to human health and the environment. Health Canada maintains a searchable database of products: Pesticide Label Search – Health Canada |
Care must be taken with the use and storage of all insecticides and repellents. Follow all label directions. Products should not be applied to broken skin, or around nose, mouth and eyes.
Pyrethrins and pyrethroids are highly toxic to cats, while organophosphates and carbamates can be toxic to animals and people.
8.3 Pasture management
Goal: Manage pastures to minimize the accumulation and spread of pathogens and poisonous plants.
Description: Overstocking on pastures can contribute to overgrazing, dusty pasture conditions and the accumulation of pathogens which can affect horse health. Appropriate pasture management plays a significant role in managing horse parasites-such as roundworms and tapeworms-and can help reduce the use of horse wormers and insecticides. (Refer to Annex 11 for additional information on parasite management)
Best practices:
- manage pastures to prevent overstocking by adjusting stocking rates to pasture conditions;
- require all horses to participate in a parasite control program;
- rotate pastures to minimize overgrazing and to assist in reducing parasite burdens. If rotation is not possible, consider an all-weather paddock for horses to allow pasture grass to regrow, protect saturated ground and manage the amount of green grass the horses are eating;
- rotate horses and other non-susceptible livestockFootnote 22 that consume about the same amount in the same pasture during the height of parasite exposure (summer months);
- only spread thoroughly composted manure on fields used for grazing, as the heat generated during composting will inactivate eggs and larvae present in the manure;
- manage the number of horses in a pasture to ensure there is even grazing of young leafy forage to minimize the development of older, taller, less desirable mature plants (roughs);Footnote 23
- provide hay when needed to keep the forage at a reasonable height (4+ inches);
- when introducing horses to pastures do it gradually and observe horses regularly;
- use cautionFootnote 24 when dragging or harrowing pastures, as this practice exposes and spreads eggs and larvae. Dragging or harrowing should only be considered during the heat of the summer when the exposed eggs and larvae will die more quickly.
- horses should be kept off the pasture post dragging or harrowing for a least a week to allow the parasite eggs and larvae to die.
- dragging or harrowing is discouraged in the cooler temperatures such as the fall. Parasites are able to survive for a longer period of time in cooler temperatures.
Additional information on pasture management:
Managing Pastures to Feed your Horse, North Carolina State University Cooperative Extension Service
Pasture Management for small strongyle control. Dr. Mary Rossano et al; University of Kentucky
Pasture Management: University of Minnesota Extension
8.4 Interior and perimeter fencing
Goal: Interior and perimeter fencing is used to safely contain horses and facilitate management of horses on the property.
Description: Fencing serves a number of purposes essential to maintaining the health and welfare of horses including: safe containment, separation of horses of different health status and age, as well as protection from predators and identification of property boundaries. Selecting the appropriate fencing materials and design should be based on the needs, intended use, durability, maintenance required, and costs.






Best practices:
Fence design, construction and placement
- align fencing needs and use with the appropriate materials and design. Consider durability (for example, lifespan and material characteristics including cracking, breaking, chipping, rotting, splintering, stretching and rusting), strength, maintenance, costs, and ease of cleaning and disinfecting if required (for example, fencing in a sick pen and for new arrivals).
- there are many materials available that are alternatives to wood fencing and that provide greater ease of cleaning and disinfection: polymer coated wood, vinyl fencing, polymer coated metal strand or mesh, high tensile metal (smooth wire, woven-wire fabric, mesh, braided polywire), electric fencing (tape, polywire and rope) and metal panel or pipe.
- enclose the property with a clearly visible perimeter fence capable of preventing the escape or intrusion by horses;
- routinely inspect the integrity of fences and gates and repair to prevent indiscriminate commingling;
- under some circumstances, there should be adequate space (at least 10 feet) between double fencing such as fenced paddocks and/or pasture areas to prevent contact between horses (Refer to Figure 10: diagram facility layout); and
- use gates and signage to restrict access to the property and areas within the facility.
Additional information on fence design:
Fence Planning for Horses: Penn State College of Agricultural Sciences Extension
Fences for Horse: University of Georgia Extension
8.5 Cleaning and disinfection of barns and equipment
Goal: Cleaning and disinfection is conducted prior to and after use, as well as in the routine maintenance of barns, stalls infrastructure and equipment.
Description: Day-to-day cleaning and disinfection is required to reduce ongoing risk of disease transmission on the farm or facility. Equipment and tools that are used to move feed or manure, or to maintain the farm or facility, particularly those used for separated or sick horses, require specialized cleaning and disinfection practices. It is important that barns, stalls, relevant infrastructure (such as water troughs and fences) and equipment are cleaned and disinfected when there is an outbreak of disease or a suspected case of disease in the herd.
Best practices:
- implement a cleaning and disinfection plan for pathogen control on equipment and environmental surfaces;
- establish cleaning and disinfection protocols and a schedule for cleaning and disinfecting the farm or facility (for example, barns, stalls, water troughs, feed and water buckets) equipment and vehicles;
- clean and disinfect common contact surfaces in paddocks and arenas (for example, gates and fences where horses congregate);
- clean and disinfect trailers, stalls and paddocks between horses and following sickness in horses;
- avoid sharing tack and equipment between horses, and clean and disinfect between horses when necessary;
- always clean before disinfecting because disinfectants are typically ineffective in the presence of organic material;
- avoid high pressure power washing as this can spread pathogens;
- use an effective disinfectant that can inactivate the relevant pathogens; and
- recognize disinfectants are chemicals with variable risks to handlers, horses and environmental surfaces.

Refer to Annex 14 on disinfectants and Annex 15 on cleaning and disinfection procedures.
Thoroughly cleaning surfaces removes the majority of pathogens and is the most important step. Only apply disinfectants to clean surfaces and follow the manufacturer's label directions.
Additional Information:
A good resource for procedures that can be applied to equine trailers: The Canadian Swine Health Board's document: Live Hog Transport Vehicle Wash/Disinfect/Dry Protocols
8.6 Barn maintenance, ventilation and wash stalls
Goal: Manage and maintain barns, buildings and wash stall areas and optimize ventilation in horse housing areas.
Description: Maintaining buildings and surfaces in good condition allows effective cleaning and disinfection which reduces the accumulation of pathogens. Good ventilation is an important consideration for the respiratory health of a horse. Ventilation is necessary to provide frequent air exchange and the even distribution of fresh air, to remove moisture and irritants (such as ammonia and particulates), and to regulate temperature. Design and drainage of wash stalls and racks is important to reduce contact among horses and between horses and environmental surfaces.
Best practices:
- ensure surfaces that horses will come into direct contact with are in good repair (i.e., not pitted and cracked);
- ensure there is adequate airflow throughout the barn;
- manage and monitor ventilation to ensure that humidity, airborne particulates and temperature are controlled to reduce their impact on horse health;
- minimize the use of interior stalls where airflow is reduced;
- review wash stall and rack design and implement measures to reduce direct contact between horses and common contact with environmental surfaces; and
- ensure wash stalls are well drained, cleaned and disinfected according to use. Wash stalls should not be drained into areas where horses are housed or pastured.
Additional information on ventilation:
Ventilation horse facilities: Penn State College of Agricultural Sciences Extension
Stall and Stable: Canadian Pony Club Education
8.7 Manure management
Goal: Manure is regularly removed, stored and disposed of in a manner that minimizes contact with the herd and prevents contamination of feed and water sources.
Description: Manure is a source of potential pathogens. Potential pathogens can remain infectious for long periods of time in the environment, and the routine removal of manure will reduce pathogen accumulation in the environment. Composting manure can provide additional benefits, including killing the eggs and immature stages of many parasites. Ensure manure storage and disposal methods comply with federal, provincial, and municipal government regulations.
Best practices:
- remove manure from horse stalls, paddocks and pastures on a regular schedule to minimize accumulation. Daily collection and removal is recommended in stalls and paddocks. Weekly and biweekly collection from paddocks and pasture can reduce the accumulation of parasites;
- dedicate tools and equipment used for manure handling to this activity. Designate equipment for areas where horses are separated from other horses. If equipment cannot be dedicated to manure removal activity or designated to specific areas, clean and disinfect the equipment between activities or areas;
- ensure manure storage capacity is sufficient for the size of the facility;
- design and locate manure storage areas to prevent contact with the herd, contamination of feed and water supplies and access by pests and wildlife;
- separate the manure storage area for resident horses from that of high risk horses to minimize opportunities for disease spread;
- compost the manure to inactivate pathogens (including parasites) if manure is to be used as fertilizer in horse pastures (or other susceptible species); and
- wash or sanitize hands and clean and disinfect footwear after handling manure.


Composting manure provides many benefits including:
- Reducing odours and the volume of manure and used bedding
- Recycling nutrients and improving soil quality when used as a soil amendment
- Killing insect and parasite eggs, pupae and larvae
- Inactivating some bacterial and viral pathogens
- Removing breeding areas for insects
- Destroying weed seeds
Additional information on manure management:
Manure and Pasture Management for Horse Owners – Alberta Agriculture and Forestry
Manure Storages for Small - to Medium-Size Horse Farms – Ontario Ministry of Agriculture, Food and Rural Affairs
Horse Stable Manure Management – Penn State Extension
Environmentally Friendly Horse Farm Through Better Manure/Waste Management - Government of British Columbia
8.8 Garbage management
Goal: Garbage, medical waste, and sharps are regularly removed and managed to minimize the transmission of pathogens.
Best practices:
- store recyclables and household and stable garbage in closed containers and dispose of regularly; and
- contain medical waste and sharps in separate approved sharps container and dispose of in accordance with local regulations. Approved sharps containers are leak-proof and puncture resistant, highly visible, designed to provide one-way entry of sharps and can be securely closed for transport. Containers can be obtained from your veterinarian, a pharmacy, a medical disposal company or medical supply store. Do not use temporary or unapproved disposal containers as they can be easily punctured or tip and spill releasing the contents.

8.9 Deadstock management
Goal: Deadstock is managed and disposed of to minimize the transmission of pathogens and contamination of the environment.
Description: Ensure the method of carcass disposal and storage complies with municipal and provincial bylaws and regulations. Depending on the region, acceptable methods of disposal may include burial, composting, cremation, rendering, natural means and landfill.
Particular care should be taken in disposing of horses euthanized by chemical solutions as they pose a significant risk because the chemicals are toxic to pets, other animals, wildlife, humans, and the environment.
Horse carcasses can be a source of pathogens, some of which survive for considerable amounts of time in the carcass. Some bacterial, fungal, and parasitic agents can replicate and increase in numbers in and on a carcass. Pests and wildlife with access to these carcasses can spread disease pathogens across the property to neighbouring facilities and to wildlife.
Disposal by natural means and burial is not permitted in all provinces, check with your provincial authority.
Euthanasia solutions (medications) are extremely potent. Even small amounts of medication in used syringes can be dangerous to animals and people. Carefully dispose of syringes and needles and wipe up any blood spatters following euthanasia to prevent human and animal contact.
Best practices:
- determine the cause of death, if not obvious, to try to rule-out contagious or infectious sources;
- if removal of the carcass and cleaning and disinfection of the area (for example, a stall or pen) is not immediately possible, prevent access by pets, pests, wildlife, other livestock, and other horses until the carcass can be moved;
- ensure carcass holding areas prevent access by pets, pests and scavengers and where carcasses are picked up by a disposal service, the location minimizes entry to horse housing areas; and
- dedicate equipment or clean and disinfect equipment used for the collection and disposal of carcasses.
Figure 10: Example of facility layout and paddock separation:

Description for image – Figure 10: Example of facility layout and paddock separation
A picture of a horse barn and outdoor paddocks surrounded by a fence to illustrate the concepts of separating horses of different health status. Clockwise from the top left of the picture: A fenced horse paddock containing a horse shelter and water trough. It is surrounded by a restricted access zone. It is labelled "Separation paddock for higher-risk horses". Separated by a grassy area to the right are two fenced paddocks with water troughs labelled "Turnout paddocks". They are each surrounded by a restricted access zone. To the far right is a building containing multiple barrels that is sited on a concrete pad. It is labelled "Feed and bedding storage". Below these areas is a large wood barn with the text "Resident horse barn". The roof of the building has been cutaway to show the inside layout. In the upper left corner of the barn is stall with hoses, water and supplies and the text "wash stall". To the right of this are sliding barn doors leading to the outside. To the right of the doors are 3 wood and metal framed horse stalls with the text: "Stalls for resident horses". To the right of this is an enclosed area with a door with the text "Feed and bedding storage". Some large wheeled garbage containers are tucked between this area and the wall of the barn. Large barn doors are open to the outside at the right of the barn. An alleyway runs the length of the barn separating the sides of the barn. On the bottom of the barn are four wood and metal horse stalls with the text "Stalls for resident horses". To the left of this is an enclosed room with the text "tack room. There is a wood and metal stall for horses at the far left lower corner of the barn. It is separated from the tack room to the right by an area of open space. There are sliding windows on both sides of the barn. The floor of the barn is concrete. Surrounding the barn is a restricted access zone. There is a biosecurity sign next to barn doors on the far right.
Separating the paddock and stabling areas for horses that have a different health status or belong to different peer groups helps minimize pathogen transmission and facilitates management of the horses on the farm or facility. The resident horse barn, turnout paddocks and separation paddock are all restricted access zones accessible through controlled access points (gates). The two-day turnout paddocks are fully fenced and separated by more than 10 feet, which prevents direct contact between horses, and each is supplied with their own watering trough. New and returning horses can be separated in a stall at the end of the barn and a turnout paddock set aside for their use.
Sick horses require the highest level of biosecurity and, ideally, should be physically separated from other horses on the property (separation barn). Restrict entry to only those people necessary for the care of these horses and require hand washing before and after entry. Dedicate coveralls and footwear specifically for this barn or clean and disinfect boots on entry and exit. Dedicate and label all tack and equipment (buckets, rakes, shovels etc.) and ensure none of it is removed and used with other horses. If a separate location is not available, a stall that is isolated from other horses within the resident horse barn can be used; however, the shared air space and close proximity to other horses can result in the inadvertent transmission of pathogens by airborne routes and other indirect methods of contact.
Section 9: Biosecurity awareness, education and training
Goal: All people attending a farm or facility or coming into contact with the horses are aware of, knowledgeable about and comply with current biosecurity protocols and practices. Standard operating procedures (SOPs) for biosecurity protocols are developed and reviewed at least annually.
9.1 Leadership and biosecurity awareness
Goal: Custodians take responsibility for ensuring the biosecurity practices are established and communicated to everyone attending a farm or facility or coming into contact with horses.
Description:
Custodians of horses and farms or facilities are ultimately responsible for ensuring the health and well-being of their horses, including establishing and communicating biosecurity protocols. On farms or facilities where horses from multiple owners commingle, there is increased risk of the introduction and spread of pathogens.
Best practices:
- custodians take responsibility for establishing and communicating biosecurity requirements;
- designate a key person to be responsible for organizing, communicating and administering the biosecurity program;
- maintain a contact list of owners, custodians, clients, farm, veterinarian, and facility workers to facilitate distribution of biosecurity materials;
- ensure horse owners and custodians take responsibility for people accessing the property on their behalf (they should provide confirmation that these individuals are aware of the biosecurity protocols and received the necessary training and education to comply with the requirements);
- maintain a copy of the biosecurity protocols in a centralized location that is accessible to all potential users; and
- provide signage applicable to good biosecurity protocols.
9.2 Education and training
Goal: All custodians and /or horse owners, their family members, clients and farm or facility workers are educated, trained and regularly updated on the biosecurity risks, protocols and results. Service providers and visitors are advised and provided an orientation on biosecurity practices.
Description:
Successful biosecurity relies on people understanding the importance, purpose and their role in the farm/facility biosecurity program and adopting the practices as part of their routine. Some individuals (owners, custodians, clients and workers) will require knowledge and training in facility specific biosecurity practices. A written biosecurity plan is fundamental to ensuring horse health and wellness. Additional knowledge on horse health, diseases and regulatory requirements is important and should be obtained from sources of valid and reliable information. Opportunities for education and training should be identified and regularly reviewed.
Training and Education Checklist:
Name:
Position/Role:
| Biosecurity training and education required (select those necessary) | Resource materials used for training | Date training completed |
|---|---|---|
| Biosecurity principles, risks, and the importance of biosecurity | ||
| Horse farm or facility management best practices manual | ||
| Biosecurity procedures and habits for regular duties | ||
| Biosecurity procedures for visitors, clients, and service providers | ||
| Biosecurity requirements and procedures for specific activities (for example, breeding, guest horse and/or new horse entry) | ||
| Introduction to horse health and diseases (basic level) | ||
| Procedures for monitoring horse health, including recognizing and reporting sickness | ||
| Contact information for health issues and emergencies, including the designated and back-up veterinarians | ||
| Record keeping including health records, reports and visitor log | ||
| Provincial and federal regulations governing or regulating infectious equine diseases | ||
| (Additional measures…) | ||
| (Additional measures…) |
There are many options for acquiring the biosecurity knowledge and training required:
- in-house orientation training sessions or meetings
- on-the-job training by working under direct supervision
- attending courses and seminars face-to-face or online
- self-study
Best practices:
- appoint a person to lead the process of developing and reviewing standard operating procedures (SOPs);
- talk to your veterinarian during the development and/or review of your procedures to ensure you target the important risks;
- incorporate the SOPs into all training and orientation;
- develop (and translate if needed) resource materials that illustrate the biosecurity protocols as part of a training and awareness program (for example, a facility handbook, posters and other factsheets/resources) for adherence and use by all property attendees;
- ensure training is provided at least annually and when there are changes to the biosecurity program;
- identify what signage is needed and where educational materials and signage should be posted;
- designate a person to be responsible for organizing and educating as necessary all property attendees and to administer the program;
- train staff and other property attendees on measures relevant to their activities and functions that address the current risks. For example, a new disease outbreak, change in horse population at the premises or increased traveling;
- maintain records of all training;
- ask potential new staff (and other property attendees) about their training, experience and approach to biosecurity with horses. Those who understand and appreciate the seriousness and potential risks of disease spread will be an asset to your facility;
- provide opportunities to discuss biosecurity issues with the designated administrator, manager or owner of the facility, boarders, guests and staff. Encourage all to discuss concerns and challenges with implementation of the biosecurity plan and provide support. Have a quick method to communicate any change in health status of a horse to the appropriate person;
- hold "team meetings" to review protocols every time a biosecurity risk is identified and an "after-the-incident" review with everyone; and
- train all horse handlers to understand and conduct a horse health check assessment, and record the results in the log book along with any concerns and follow-up.
Effective, ongoing communication is a critical component of a biosecurity plan. Changes in risks and procedures need to be communicated effectively to all participants. Feedback is critical to developing good techniques.
Section 10: Farm and facility location, design, layout and renovations to existing facilities
Goal Good planning and assessment of your farm or facility from a biosecurity perspective can help reduce the risk of the spread of disease or introduction of disease to your property. A diagram of the farm or facility layout can be helpful to assess the high and low risk areas, including the traffic flow, visitor areas, manure management and fencing needs for pathways, as well as prevailing winds and water run-off.
Description:
Biosecurity principles should be included when designing or re-designing the property layout and environment. Often small changes may be implemented that can have a positive impact. Priority areas for the design and layout of a facility include: geography, topography, and traffic flow with end use in mind. For information on sound management and welfare practices of horse housing and care refer to the Code of Practice for the Care and Handling of Equines.
10.1 Geography
The overall geography of the area and of the facility should be assessed from the point of view of limiting the spread of disease and minimizing its introduction to the facility. Constructing new facilities in areas that are less densely populated with horses and livestock can reduce the risk of exposure to pathogens. Assess needs and balance benefits relative to access to veterinary services, feed suppliers, and other equine event complexes that may be located in the surrounding area.
| Considerations and best practices | Notes |
|---|---|
| New Facilities – Construct a sufficient distance from other equine facilities, event complexes, commingling facilities or livestock facilities so as to minimize the airborne transmission of infectious diseases. | |
| Acquire knowledge of surrounding industries prior to building a facility to minimize the impact from potential sources of contamination and hazards (biological, chemical, physical). | |
| Determine the proximity to equine veterinary clinics, event, and commingling locations so as to minimize transport stress and/or exposure to other animals. | |
| Obtain information of identified regional diseases and their modes of transmission. |
10.2 Topography
Incorporate natural surface features (topography) in the design of the site. This may influence the overall use of the property, location of buildings, turnout areas, pastures and other necessary infrastructure of your farm or facility. The slope and type of soil will affect drainage, ease and cost of grading and building, pasture quality and footing for horses. Trees and hills can provide protection from sun, wind, and inclement weather and affect airflow in barns. Ponds and streams may reduce useable area, attract wildlife and pests and affect drainage.
| Considerations and best practices | Notes |
|---|---|
| Select a location that is slightly elevated, provides adequate drainage and suitable ground cover for pasture and a base for stables. | |
| Determine if there are areas where standing water can accumulate and assess ways to minimize this risk. | |
| Determine if measures will be necessary to prevent water run-off that would cause flooding of barns, farms and facilities. | |
| Consider risks of disease if the paddocks or turn out areas run through wooded areas that may contain tick species that harbour pathogens such as Borrelia burgdorferi (the cause of Lyme disease). | |
| Assess the area to ensure there is sufficient space for manure storage and/or composting. Placement needs to allow separation from the barn and feed storage but still be accessible for daily cleaning out of manure, soiled bedding and feed as well as consideration for access by vehicles and large equipment for removal of manure and/or compost. |
10.3 Layout
The layout of the site affects the ease and efficiency of day to day operations and the ability to implement effective biosecurity practices. The layout must account for the intended number of horses and allow for expansion as needed. Being able to separate horses from different peer and risk groups is important, as is the ability to minimize contamination of housing, feed, water and bedding.
| Considerations and best practices | Notes |
|---|---|
| Locate the manure storage area to prevent leeching or run off into horse housing areas, ditches, water sources, and surface water reservoirs such as creeks, ponds, rivers and lakes. | |
| Ensure all access points to the barn are secure and visible. | |
| Minimize possible nose-to-nose contact over fences (for example, double fencing, see figure 10), particularly in high-risk zones. | |
| Ensure the farm or facility layout is designed to allow for the separation of peer and risk groups. | |
| Locate horse loading and unloading areas in an area to minimize vehicle traffic onsite. |
10.4 Traffic flow
The uncontrolled movement of people, horses, equipment and materials on a farm or facility can quickly and easily spread pathogens. Identifying and planning traffic flows can reduce this risk.
| Considerations and best practices | Notes |
|---|---|
| Assess pathways for the movement of vehicles, supplies and horses. If possible, design the layout to minimize contact among horses. Designate parking areas (and post signage) for suppliers, veterinarians, farm workers, and visitors to help to reduce spread of disease. | |
| Consult first responders to ensure facility design is suitable for access in emergency situations. | |
| Control and manage access to your property including but not limited to visitors, horses, other livestock, pets and wildlife. | |
| Post highly visible biosecurity signage. | |
| Ensure that the service providers (for example, utility providers, feed deliveries, veterinarians, and farriers) have dedicated places to park that are in low-traffic areas. | |
| Manage the separation of horses and people involved in different horse disciplines (for example, facilities that run riding schools should keep foot traffic and school horses separate from show and/or other client horses). | |
| House horses assigned to one trainer together and separate from those of another trainer or discipline. | |
| Designate a trailer parking area. |
10.5 Design of new physical structures or renovation to an existing physical structure
There are many types of structures that are used to house horses, including structures that that were designed for other livestock (for example, renovated cow barns). The structure needs to be assessed from the position of equine biosecurity, as the needs of other species may be very different than those required for horses. The following are best practices in the design of a new facility or renovating an existing structure to support the implementation of equine biosecurity.
| Considerations and best practices | Notes |
|---|---|
| When repairing or enlarging the facility, select building materials that are smooth, non-porous, durable and easy to clean and disinfect (for example, metal, sealed concrete and some plastics). This is especially important for exposed surfaces that horses will have frequent contacts with such as walls, dividers, stall surfaces and floors. | |
| Seal wooden surfaces (such as fences, barn and building walls) with multiple coats of a non-toxic marine grade enamel paint or urethane to provide a surface that can be more easily cleaned and disinfected. Avoid sealing surfaces that horses may chew or ingest. | |
| Select building materials that will not shatter or splinter when kicked by horses. | |
| Ensure there are a sufficient number of taps and sinks for cleaning and hand washing. Install hand sanitation stations for visitors and staff and post notices on acceptable procedures (for example, written protocols for cleaning and disinfection). | |
| Ensure there is adequate subsurface drainage to remove waste water and storm water from within and around barns, buildings and paddocks. | |
| Develop a transition area – A location where all persons can change footwear and clothing before entering horse housing areas especially in areas where they may pose higher biosecurity risks. | |
| Install window screens to keep flies and mosquitoes out of barns and regularly inspect for pest infestation and areas that may encourage breeding of pests (for example, standing water or piles of material or debris). | |
| Ensure there is a stall and a pasture for the separation of a new or sick horse that keeps the horse and its equipment separate from the resident horses. | |
| Ensure that water bowls, mangers, feeders and buckets can be regularly cleaned and/or disinfected. | |
| Use non-slip flooring. | |
| Ensure lighting is available that is appropriate to the needs and out of reach of horses. | |
| Ensure air circulation is sufficient throughout the horse housing areas to provide a supply of fresh air and minimize dust, odour and humidity. | |
| Ensure temperature within the housing areas can be managed for comfort and to prevent moisture buildup in enclosed areas. | |
| Ideally, store straw and hay in a separate building or away from the horses with only a 2-3 day supply being brought into the barn/stable area. | |
| Ensure stalls are large enough to accommodate a horse lying down and provide ample head room and space to easily get to their feet (adequate lunge space). It is also important to consider possible dead stock management and access for removal when this becomes necessary. Refer to the Code of Practice for the Care and Handling of Equines. | |
| Construct and employ fencing and gates to maintain optimal separation between animals (for example, while at pasture, in transit to barns, or between vehicles and animals). | |
| Separated paddocks for new, injured or sick horses can be set up (permanently or temporarily) with defined and separate access. | |
| Use fencing to keep horses out of creeks and ponds and to prevent access to other high risk areas. |
Annex 1: Development of the user guide and acknowledgements
The user guide was developed through a partnership of Equestrian Canada and the CFIA in collaboration with Agriculture and Agri-Food Canada. An advisory committee representing a broad cross-section of the industry comprised of equine owners, subject matter experts, provincial government officials, representatives from regional and sector-specific equine industry organizations, academics, and the public sector, provided invaluable guidance throughout the process.
The user guide augments the National Farm and Facility Level Biosecurity Standard for the Equine Sector and provides additional details and guidance on achieving the biosecurity goals.
| Representative | Organization/Affiliation |
|---|---|
| Bill desBarres | Alberta Equestrian Federation and Horse Welfare Alliance of Canada |
| Dr. Adam Chambers | Ontario Racing Commission |
| Dr. Alison Moore | Ontario Ministry of Food, Agriculture and Rural Affairs |
| Dre Chantal Proulx | Ministère de l'Agriculture, des Pêcheries et de l'Alimentation du Québec |
| Dr. David Paton | Equine Private Practitioner (British Columbia) |
| Dr. Darrell Dalton | Alberta Veterinary Medical Association |
| Dorothy Willows | Horse Industry Association of Alberta |
| Dr. Daniel Schwartz | Canadian Food Inspection Agency |
| Gayle Ecker | Equine Guelph, University of Guelph |
| Isabelle Breton | Horse owner and biologist |
| Jack de Wit | Equestrian Canada |
| Kathryn Tonita | Saskatchewan Ministry of Agriculture |
| Les Burwash | Alberta Agriculture and Rural Development |
| Dr. Mary Bell | Equestrian Canada and Equine Private Practitioner |
| Dr. Patricia Pentney | Canadian Food Inspection Agency |
| Renée Lévesque | Cheval Québec |
| Dr. Ron Clarke | Former Equine Private Practitioner (Alberta) |
| Dr. Ross A. McKague | Equine Private Practitioner (Manitoba), Manitoba Jockey Club and Assiniboia Downs (racetrack) |
| Sandra Conrad | Equestrian Canada (Atlantic Representative) and Nova Scotia Equestrian Federation |
| Dr. Scott Weese | Ontario Veterinary College |
| Dr. Susan Raymond (alternate for Gayle Ecker) | Equine Guelph, University of Guelph |
| Virginie Rochet | Sector Specialist, Agriculture and Agri-Food Canada |
| Dr. Wayne Burwash | Equine Private Practitioner (Alberta) |
Annex 2: Important infectious diseases of horses in Canada
Selected Horse Diseases: The following table provides a list of important equine diseases that are a potential risk to the health of the Canadian equine herd. Many of the disease pathogens are already present in Canada, while others pose a risk through the importation of horses, semen, embryos, contaminated equipment or through international travel to equestrian events. Legend B (bacterial), F (fungal), P (parasite), V (viral). This is not a complete list and does not include internal parasites (Refer to Annex 12).
| Name | Pathogen | Type | Horses can infect people | Route of transmission Direct (contact) | Route of transmission Indirect (fomite) | Route of transmission Aerosol/airborne | Route of transmission Vector | Route of transmission Ingestion | Other | Comment |
|---|---|---|---|---|---|---|---|---|---|---|
| Anthrax | Bacillus anthracis | B | Yes | X | X | X | X | |||
| Aspergillosis | Aspergillus spp | F | No | X | X | X | ||||
| Botulism | Clostridium botulinum | B | No | X | ||||||
| Brucellosis | Brucella spp | B | Yes | X | X | X | Reproductive | |||
| Clostridium difficile infection | Clostridium difficile | B | Maybe | X | ||||||
| Coccidioidomycosis | Coccidioides immitis and C. posadasi | F | Yes | Contact with soil. Not horse-to-horse | ||||||
| Contagious Equine Metritis (CEM) | Taylorella equigenitalis | B | No | Reproductive | Not currently present in Canada | |||||
| Coronavirus | Equine coronavirus | V | No | X | ||||||
| Cryptococcosis | Cryptococcus neoformans, C, gattii | F | No | Environmental. Not horse-to-horse. | ||||||
| Cryptosporidiosis | Cryptosporidium parvum | P | Yes | X | ||||||
| Dourine | Trypanosoma equiperdum | P | No | Reproductive | Not currently identified in Canada | |||||
| EEE | Eastern equine encephalomyelitis virus | V | No | Mosquito | ||||||
| Equine granulocytic anaplasmosis | Anaplasma phagocytophilum | B | No | Ixodes ticks | ||||||
| Equine herpesvirus type 1 abortion | Equine herpesvirus type 1 (EHV-1) | V | No | X | X | X | X | |||
| Equine herpesvirus type 1 neurological disease (myeloencephalopathy) | EHV-1 | V | No | X | X | X | X | |||
| Equine herpesvirus type IV | EHV-4 | V | No | X | X | X | ||||
| Equine infectious anemia | Equine infectious anemia virus | V | No | Biting flies | Cross-contamination of blood. Aerosolized blood. | |||||
| Equine protozoal myeloencephalitis (EPM) | Sarcocystis neurona | P | No | X | Associated with exposure to feces from opossums and some the other small mammals | |||||
| Equine viral arteritis (EVA) | Equine viral arteritis virus | V | No | X | X | Reproductive | ||||
| Influenza | Equine influenza virus | V | No | X | X | X | ||||
| Glanders | Burkholderia mallei | B | Yes | X | X | X | ||||
| Leptospirosis | Leptospira interrogans | B | Maybe | X | X | Contaminated water major source | ||||
| Lice (pediculosis) | Haematopinus asini, Bovicola equi | P | No | X | X | |||||
| Lyme disease | Borrelia burgdorferi | B | No | Ticks (Ixodes spp) | ||||||
| Mange | Chorioptes equi, Sarcoptes scabiei, Demodex equi | P | Yes for Sarcoptes | X | X | |||||
| MRSA | Methicillin-resistant Staphylococcus aureus | B | Yes | X | X | |||||
| Piroplasmosis | Babesia caballi, Theileria equi | P | No | Certain ticks | Blood | |||||
| Potomac horse fever | Neorickettsia risticii | B | No | Aquatic insects | Ingestion. Mainly from surface water | |||||
| Rain scald/rain rot | Dermatophilus congolensis | B | No | X | X | |||||
| Rhinovirus | Equine rhinovirus | V | No | X | X | |||||
| Rhodococcus equi pneumonia | Rhodococcus equi | B | Rarely | X | ||||||
| Ringworm | Trichophyton equinum, Microsporum canis | F | Yes | X | X | |||||
| Salmonellosis | Salmonella sp | B | Yes | X | ||||||
| Strangles | Streptococcus equi equi | B | No | X | X | |||||
| Venezuelan equine encephalitis (VEE) | Venezuelan equine encephalitis virus | V | Yes | Mosquitoes | Not currently identified in Canada | |||||
| Vesicular stomatitis | Vesicular stomatitis virus | V | No | X | Insects. Mainly sandflies and black flies. | Not currently identified in Canada | ||||
| Western equine encephalitis (WEE) | Western equine encephalitis virus | V | No | Mosquitoes | ||||||
| West Nile encephalitis | West Nile virus | V | No | Mosquitoes |
Annex 3: Self-evaluation checklist for risk assessment
Equine farm or facility level biosecurity self-assessment tool
The objective of the self-assessment is to identify areas of risk and identify appropriate biosecurity actions to develop your site-specific biosecurity plan.
For the purpose of this self-assessment, separation is defined as using physical barriers to prevent direct contact between horses. Separation is a management tool to minimize the risk of introduction and spread of disease. Other terminology such as isolation and quarantine is commonly used for specific purposes of separation (see separation in the glossary for additional information on other terminology).
Date of assessment: ![]()
Components of a biosecurity plan
| 1a) Owner, farm or facility identification and other important contact information. | Name: Location (Physical and Geographic Information System – GIS): Contact person: Emergency contact (people and numbers): Veterinarian: Farrier: Police: Fire: Ambulance: Other: |
| 1b) Identified resources and communication networks to adjust your biosecurity plan and training protocols to potential risks in your area and region. |
| Biosecurity activities 2a) All resident horses. Do you… | Yes | No | Sometimes | If no, identify biosecurity measures that could be implemented on your farm or facility that would minimize the risk or concern. |
|---|---|---|---|---|
| have a veterinarian that is familiar with your farm or facility and the herd health practices? | ||||
| have an agreement in place for horses under the care of individuals other than the owner, that provides for an immediate response in the event of potential welfare impacts or disease? | ||||
| have a preventive health program for resident horses? | ||||
align new horses to the farm or facility preventive health program either:
|
||||
align new horses to the farm or facility preventive health program:
|
||||
| monitor and inspect horses daily for signs of sickness? | ||||
| separate horses with consideration to age, health status, use and social well-being? | ||||
| have established (and written) disease response and emergency protocols?; and | ||||
|
||||
| maintain health records of horse treatments? | ||||
| obtain a veterinary diagnosis for horses that appear to have died from an infectious disease or an unknown cause? |
| Biosecurity activities 2b) Managing sick or ill horses. Do you… | Yes | No | Sometimes | If no, identify biosecurity measures that could be implemented on your farm or facility that would minimize the risk or concern. |
|---|---|---|---|---|
| have a separate stall and/or paddock for sick horses that prevents contact with other horses? | ||||
| work with healthy horses before attending to sick? | ||||
| wear gloves and protective clothing when handling sick horses? | ||||
| wash your hands after handling sick horses? | ||||
| disinfect footwear (if boot covers are not available) after working with sick horses? | ||||
use designated or dedicated equipment:
|
||||
use designated or dedicated equipment:
|
||||
clean and disinfect equipment used:
|
||||
clean and disinfect equipment used:
|
| Biosecurity Activities Do you… | Yes | No | Sometimes | If no, identify biosecurity action points that could be implemented on your farm or facility that would minimize the risk or concern. |
|---|---|---|---|---|
| require validation of the health status of a horse prior to accepting arrival at the farm or facility? (This includes a review of health records to ensure deworming and vaccination status are consistent with the resident herd). | ||||
| have a procedure and written agreement to align the health status of horses prior to arrival if their health status is not consistent with the resident herd? (For example, vaccinate as indicated or align to the facility management deworming program). | ||||
| have a separate stall and/or paddock that prevents contact with resident horses for new arrivals, returning and visiting horses? | ||||
| Or are there other protocols that prevent contact with resident horses? | ||||
| separate new additions or returning horses from the resident herd upon arrival? | ||||
| require the equipment for visiting horses (tack, grooming, feed and water buckets) to be designated to an individual horse, and be cleaned and disinfected prior to arrival at your farm or facility? | ||||
| validate the health status of horses visiting for short term activities (not housed overnight)? | ||||
| Keep these horses separate from the resident herd at all times? | ||||
| provide event managers permission to take measures to minimize disease risks if disease is identified in your horse or a participant's horse while at an event? | ||||
| clean and disinfect trailers prior to use? |
| Biosecurity activities Do you… | Yes | No | Sometimes | If no, identify biosecurity action points that could be implemented on your farm or facility that would minimize the risk or concern. |
|---|---|---|---|---|
| have established criteria that must be met to permit access to your farm or facility? (This includes criteria for equipment, horses, vehicles and people). | ||||
| have visible signage that identifies access and biosecurity considerations? | ||||
| restrict the access of visitors and visiting horses to only those areas that are required for their activities with biosecurity considerations? (For example, their access is limited to only the areas that are necessary). | ||||
| require everyone to wash and sanitize their hands before and after contact with horses? | ||||
| limit farm and facility access to only essential people, equipment, vehicles, inputs, and horses? | ||||
| have access points that are secured or monitored to increase compliance to biosecurity protocols? | ||||
| have a perimeter fence that encloses the farm or facility to keep resident horses secured and other animals out? | ||||
| ensure fences and gates are maintained to prevent unplanned commingling of your horses with those from another operation? | ||||
| have a clearly identified parking area that is separate from the controlled access area? |
| Biosecurity activities Do you… | Yes | No | Sometimes | If no, identify biosecurity action points that could be implemented on your farm or facility that would minimize the risk or concern. |
|---|---|---|---|---|
| have a visitor log that is available to record visitors on the farm? | ||||
And:
|
||||
| have a location (station) for hand washing with hand sanitizer, paper towels, and signage indicating recommended procedures for bio-safety? | ||||
| clean and disinfect stalls regularly and between horses? | ||||
| clean and disinfect wash stalls frequently in accordance with use? | ||||
And:
|
||||
| designate or dedicate equipment for specified activities (for example, dedicate shovels for manure handling from resident healthy horses)? | ||||
| designate or have specific equipment to be used only for each individual horse? (if not, do you clean and disinfect equipment between horses)? | ||||
| have an established pest and parasite control program in place? | ||||
And:
|
||||
| test and treat water if indicated? | ||||
| clean and disinfect water distribution equipment regularly (weekly) between different horses? | ||||
And:
|
||||
| source feed and bedding from reputable providers with verifiable quality assurance programs in place? |
| Biosecurity activities Do you… | Yes | No | Sometimes | If no, identify biosecurity activities that could be implemented on your farm or facility that would minimize the risk or concern. |
|---|---|---|---|---|
| develop biosecurity standard operating procedures with input from your veterinarian and are they specific for your farm or facility? | ||||
| have a designated trained person to review and update the biosecurity standard operating procedures? | ||||
| have a training program for staff and all personnel that is based on the farm or facility biosecurity standard operating procedures? | ||||
| provide the training program to all staff; | ||||
| And is it reviewed, and updated as required? | ||||
| have all training and procedures documented and posted for easy reference by staff and personnel? |
| Biosecurity activities Do you… | Yes | No | Sometimes | If no, identify biosecurity activities that could be implemented on your farm or facility that would minimize the risk or concern. |
|---|---|---|---|---|
| engage a diversity of expertise in the development of the design? | ||||
| consider the effects of local and regional geography in the evaluation of biosecurity implementation? | ||||
| consider the topography of the development site in the evaluation of biosecurity implementation? | ||||
| base (consider) the layout of the facility on the implementation of biosecurity to facilitate separation and manage the traffic flow of people, equipment, horses, and inputs? |
Annex 4: Conducting a horse health check

To optimize health and welfare, you should know how to assess basic horse health. Knowing the normal range of your horse's vital signs and physical condition and their standard character, behaviour and activity level is necessary to determine what is abnormal and might indicate sickness. Subtle health changes can be easily missed, particularly if you are not looking for them.
Performing a horse health check does not replace the need and benefits of a physical exam by a veterinarian. The health check provides an early warning of a potential health issue. The information will assist your veterinarian in determining the severity of the health issue and establish the priority of attending to your horse.
Record the results of your horse health check.
Perform the horse health check any time you believe there is a change in the health status of your horse. Check your horses daily when attending competitions and weekly when at your home farm or facility.
Equipment
- digital thermometer;
- lubrication for the thermometer;
- watch capable of displaying seconds;
- stethoscope;
- gloves and supplies to clean and disinfect your hands and equipment before and after the exam.
| How to conduct a horse health check
Table Note 25
Table Note 26 Health checks include observing your horse at rest and in motion, from a distance and up close. |
|---|
|
From a distance – Assess demeanor and behaviour.
|
Appetite and water intake
|
Manure and urine
|
Up close
|
Temperature
|
Heart rate
|
Respiration
|
Mucous membranes and capillary refill time
|
Examine the head |
Abdominal/Intestinal sounds
|
Table Notes
- Table Note 25
- Table Note 26
- Table Note 27
- Table Note 28
Annex 5: Horse Health Exam Record
Horse Exam Record
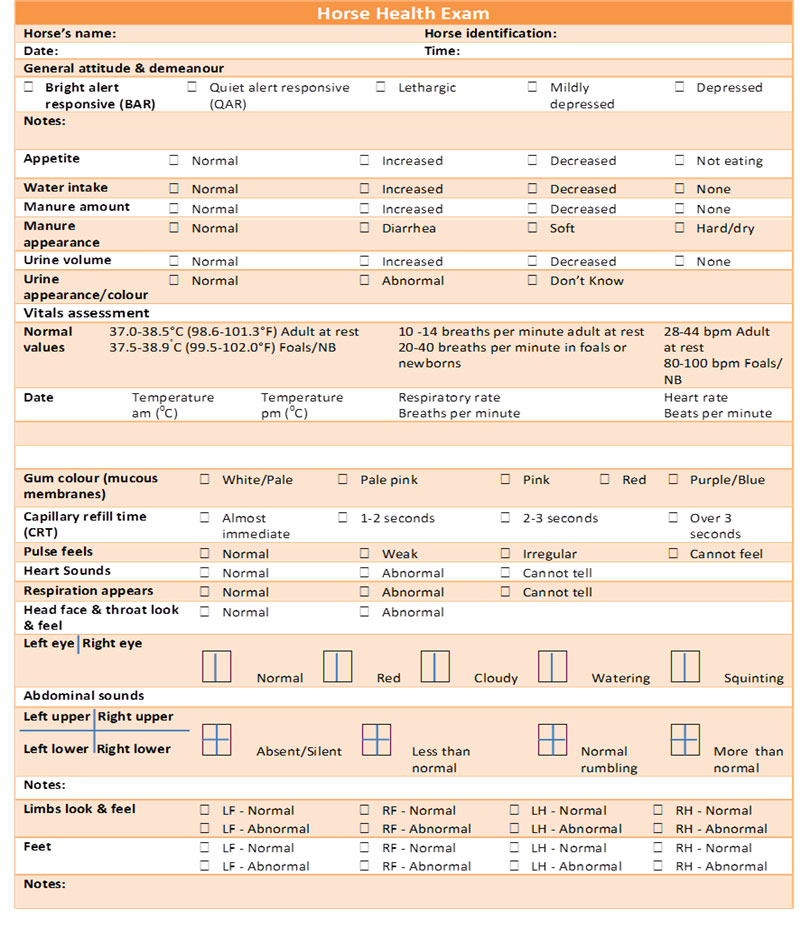
Description for image – Horse Exam Record
The picture is of a table to record a horse health exam. The rows of text in the table are:
Horse Health Exam
Horse's name, Horse identification
Date and Time:
General attitude & demeanour
Bright alert responsive (BAR), Quiet alert responsive (QAR), Lethargic, Mildly depressed, Depressed
Notes:
The next section of the table pertains to food and voiding and contains rows that ask:
Appetite: Normal, Increased, Decreased, Not eating
Water intake: Normal, Increased, Decreased, None
Manure amount: Normal, Increased, Decreased, None
Manure appearance: Normal, Diarrhea, Soft, Hard/dry
Urine volume: Normal, Increased, Decreased, None
Urine appearance/colour: Normal, Abnormal, Don't Know
The next section of the table contains information on the normal values of vitals such as temperature, respiratory rate and heart rate and a place to record information:
Vitals assessment
Normal values: 37.0-38.5°C (98.6-101.3°F) Adult at rest and 37.5-38.9°C (99.5-102.0°F) Foals/NB
10 -14 breaths per minute adult at rest, 20-40 breaths per minute in foals or newborns
28-44 bpm Adult at rest, 80-100 bpm Foals/ NB
Date: Temperature am (°C), Temperature pm (°C), Respiratory rate, Breaths per minute, Heart rate Beats per minute
Gum colour (mucous membranes): White/Pale, Pale pink, Pink, Red, Purple/Blue
Capillary refill time (CRT): Almost immediate, 1-2 seconds, 2-3 seconds, Over 3 seconds
Pulse feels: Normal, Weak, Irregular, Cannot feel
Heart Sounds: Normal, Abnormal, Cannot tell
Respiration appears: Normal, Abnormal, Cannot tell
Head face & throat look & feel: Normal, Abnormal
Left eye, Right eye: Normal, Red, Cloudy, Watering, Squinting
Abdominal sounds
Left upper, Right upper, Left lower , Right lower: Absent/Silent, Less than normal, Normal rumbling, More than normal
Notes:
Limbs look & feel: LF – Normal, LF - Abnormal, RF – Normal, RF – Abnormal, LH – Normal, LH – Abnormal, RH – Normal, RH - Abnormal
Feet: LF – Normal,LF – Abnormal, RF – Normal, RF – Abnormal, LH – Normal, LH – Abnormal, RH – Normal RH - Abnormal
Notes:
Annex 6: Vitals Exam Record

Description for image – Vitals Exam Record
Sample form for vitals exam record
The form heading reads: Vitals Exam Record – When at competition or any commingling venue.
The heading is followed by a paragraph: Monitor rectal temperature twice per day. If temperature exceeds normal value, perform a horse health check and contract your veterinarian as necessary.
The form then contains two fields:
- Horse Name
- Horse Identification
The rest of the form is a table used to collect the following information:
- Under the header Normal values: Date
- Under the header 37.0-38.5°C (98.6-101.3°F) Adult at rest , 37.5-38.9°C (99.5-102.0°F) Foals/Newborn:
- Temperature am (°C)
- Temperature pm (°C)
- Under the header 10-14 breaths per minute Adult at rest, 20-40 breaths per minute in foals or newborns:
- Respiratory rate (Breaths per minute)
- Under the header 28-44 bpm Adult at rest, 80-100 bpm Foals/Newborn
- Heart rate in Beats per minute (bpm)
Annex 7: Sample horse event participant declaration
Event information
Event name:
Event location:
Event date(s):
Information for contact person
Name of person in charge of horse(s) at the event:
Address:
Email address:
Home phone #:
Cell phone #:
Truck licence plate #:
Trailer licence plate #:
| Horse's name | Breed | Identification (colour, markings, brand, electronic identification) | Sex | Age | Resting horse temperature (<38.5°C) |
|---|---|---|---|---|---|
| Address of property (premises identification) from which the horse was moved to the event: | |
|---|---|
| Address of property (premises identification) to which the horse will move after the event (If different from above): |
Alternate contact information (For other individuals affiliated with horses):
Name:
Cell phone #:
Name:
Cell phone #:
Horse health declaration:
I, ![]() , declare that the horse(s) named above has/have:
, declare that the horse(s) named above has/have:
- been in good health;
- been eating normally;
- body temperature(s) below 38.5°C (101.3°F);
- and not shown signs of infectious disease for the three (3) days preceding arrival at this event including transport.
Signature: ![]() Date:
Date: ![]()
(Complete a separate form for different owners.)
For event officials' use only:
Date and time of arrival: ![]() Event official initials:
Event official initials: ![]()
Date and time of departure: ![]() Event official initials:
Event official initials: ![]()
Annex 8: Sample letter to participant
Dear participantFootnote 29,
Protecting the health and welfare of your horse and other horses at this event is of primary importance to event management. Biosecurity measures are being implemented to reduce the risk of the introduction and spread of infectious diseases.
All horses entering the grounds will be subject to examination by event officials and/or designated representatives. Such examinations are to determine the horse's health status. If after such examination, an official believes the health of a horse places other horses at risk, the officials may separate and restrict the movements of the horse(s) and others that may have been infected or exposed, or, if necessary, require horse(s) to be removed from the event premises.
All participants must agree to fully cooperate with examining officials and abide by their decisions and instructions. Failure to comply with officials shall be grounds for immediate expulsion of the participant from the grounds and potential disciplinary action(s) by governing bodies.
The equine health entry requirements for this event include: (event manager may choose one or more and delete others)
- Horses displaying obvious signs of clinical disease, such as fever, abnormal nasal discharge, consistent frequent coughing, neurologic signs of ataxia or significant hind limb weakness are not permitted to enter the event grounds.
- Event no fever policy:
- Each horse entering the premises must have documentation attesting to having body temperatures monitored
 daily with no readings above 38.5°C (101.3°F) for adult horses or for foals 38.9°C (102.1°F) at rest or for
daily with no readings above 38.5°C (101.3°F) for adult horses or for foals 38.9°C (102.1°F) at rest or for  days before arrival at the event premises.
days before arrival at the event premises. - Show officials will obtain a body temperature of all horses at the time of arrival to the event premises and all horses will be subject to periodic inspection by event officials during the event.
- Horse owner/custodians will monitor and document on a log the body temperature of their horse(s)
 times a day during the event.
times a day during the event.
- Each horse entering the premises must have documentation attesting to having body temperatures monitored
- Health certification policy: Horse owner/custodians must present to event officials at the time of arrival to the event premises, proof (a health certificate) of a veterinary inspection conducted within the past
 hours indicating the horse is free of infectious and contagious diseases.
hours indicating the horse is free of infectious and contagious diseases. - Event participation declaration: (Refer to Annex 7 for Sample Horse Event Participation Declaration)
- Horse owner/custodians must sign a health certification statement verifying that the horse(s) has/have been healthy with no signs of infectious disease for the preceding
 days and a body temperature below 39°C (102°F) during the past
days and a body temperature below 39°C (102°F) during the past  hours before arrival at the event premises.
hours before arrival at the event premises. - Horse owner/custodians must provide event officials with the address of the premises where each horse was located immediately before arrival at the event and the address of the intended premises of destination for each horse following departure from the event premises.
- Horse owner/custodians must sign a health certification statement verifying that the horse(s) has/have been healthy with no signs of infectious disease for the preceding
In addition to the above requirements, participants are asked to comply with the following:
- Dogs are not permitted on the event premises OR All dogs on the event premises must be kept on a leash;
- Stable horse(s) only in assigned stall;
- Restrict your access to only your assigned housing/stabling area;
- Limit horse-to-horse contact;
- Limit horse-to-human-to-horse contact;
- Do not share equipment between horses from different owners (tack, water buckets, brushes, and rags etc.);
- Do not submerge the end of water hoses in water buckets;
- Do not allow horses to drink directly from a water hose;
- Avoid tying horses to fences or gates near the competition area;
- Cover (store) all feed and hay to prevent access by pests, birds or other animals;
- Monitor your horse frequently for signs of disease during the event;
- Immediately report any sick horse(s) to event officials;
- Thoroughly clean and disinfect all equipment before use at the home premises;
- Separate and monitor all horses upon return to the home premises.
In the event of an emergency or infectious disease incident at the event, all participants and horses will remain at the event venue until event officials provide clearance for departure from the premises. If an infectious disease is identified event officials will evaluate individual horse disease exposure risk and provide horse owner/custodians with follow up disease monitoring instructions. If movement restrictions are put in place, each horse owner/custodian is responsible for the care and maintenance of their respective horse(s) on the premises.
We appreciate your compliance with event management's efforts to maintain biosecurity and the health of all horses at the upcoming event.
Sincerely,
(Signature)
Annex 9: Incoming horse protocol and checklist
| Requirements | Notes | Completed |
|---|---|---|
| Ensure your farm or facility has sufficient space to accommodate additional horses | ||
Establish separation area for incoming horses that prevents direct nose-to-nose contact between horses.
|
||
| Dedicate equipment for use with separated horses; or Clean and disinfect equipment before and after use with separated horses. |
||
| Restrict access to separated horses and post biosecurity signage. | ||
If purchasing horses:
|
||
| Ensure horses are identifiable – Record distinct markings, tattoos, brand, or microchip. | ||
| Request proof of veterinary clinical physical exam with negative findings for infectious diseases within previous 7 ( |
||
| Request and review vaccination and deworming history. | ||
Obtain proof of EIA test with negative results within past (
|
| Requirement | OR | Requirement | Notes | Completed |
|---|---|---|---|---|
Horses vaccinated prior to arrival within the past (
|
OR | Horses vaccinated on arrival against:
|
Prior Or On | |
Horses vaccinated prior to arrival within the past (
|
OR | Horses vaccinated on arrival against:
|
Prior Or On |
| Requirements | Notes | Completed |
|---|---|---|
| Conduct fecal egg count and deworm horses as appropriate. | ||
| Request and review medical records. | ||
Separate incoming horses for:
|
||
| Monitor the health of new horses daily, including rectal temperature and record results in a medical record. | ||
| If signs of sickness are observed in new horses, ensure clothing and footwear is changed and hands are washed after contact with horse. Conduct a horse health check and contact your veterinarian to establish a diagnosis. | ||
Additional notes: |
Annex 10: Additional guidance on vaccination
Vaccination is the primary means for increasing resistance to specific infectious pathogens. Safe and effective vaccines have been developed for a number of equine diseases and when used appropriately can prevent or minimize the severity and duration of disease. Discuss a vaccination program with your veterinarian to tailor it to the specific risks and requirements of your horse(s). With your veterinarian, review the disease risks, identify which diseases to vaccinate against and determine a schedule to maximize the benefits during periods of greatest risk.
Determining which diseases to vaccinate against should be based on:
- risk of disease. For example:
- likelihood of exposure (consider feeding and horse management practices);
- geographic location;
- frequency of travel and contact with horses from different premises.
- consequences of disease;
- potential for adverse vaccine reactions; and
- vaccine efficacy and anticipated benefits.
Additional factors influencing vaccination include the horse's age, health status, vaccination history, travel history, and previous responses to vaccines.
Trying to develop a one-size-fits-all vaccination protocol for all horses is impractical and runs counter to the objectives of maximizing disease resistance. The American Association of Equine Practitioners (AAEP) has developed a series of guidelines and protocols for vaccination. They categorize vaccines as either "Core" or "risk-Based".
| Core vaccines | Risk-based vaccines |
|---|---|
|
|
Table Notes
- Table Note 30
-
American Association of Equine Practitioners Vaccination Guidelines
- Table Note 31
-
Equine Guelph, University of Guelph, Vaccination Equi-Planner - Vaccination Guidelines
- Table Note 32
-
Ibid
While vaccination is a critical component of maintaining horse health, vaccination does not provide a complete guarantee against disease occurring. Many factors affect the outcome following disease exposure (refer to the disease triad). Good biosecurity, animal husbandry and management practices are necessary to maximize the benefits of vaccination.
For a vaccine to be effective it must be stored and administered according to label directions. Some vaccines require more than one does given at specific intervals in order to be effective. Your veterinarian is the best resource for vaccine recommendations specific to your horse.
Storing and handling vaccines
- read and follow the manufacturer's label directions for storage;
- ensure vaccines requiring refrigeration are stored at the proper temperature; vaccines should not be allowed to freeze. Avoid storing in the door, bins or drawers of the refrigerator as the temperatures often fluctuate in these locations;
- monitor the temperature of refrigerators storing vaccines with a digital thermometer;
- protect vaccines from sunlight exposure; sunlight can breakdown components of the vaccine; and
- monitor expiry dates and rotate older vaccines into use ahead of newer products.
Administering vaccines
- read and follow the manufacturer's label directions for administering;
- for vaccines that require reconstituting, mix with the proper liquid (diluent) at the correct volume and temperature;
- do not mix vaccines with other vaccines or medications in the same syringe or applicator;
- only reconstitute the amount of vaccine that will be used immediately; do not store reconstituted vaccine. Reconstituted vaccines are often not stable and will not be effective if stored;
- use a new needle and syringe for each animal;
- administer vaccine by the proper route (for example, intramuscular, subcutaneous, intranasal) using correct technique;
- do not reduce or split the dose of vaccine between animals;
- properly dispose of needles, syringes and used vaccine containers;
- maintain a vaccination record including date, vaccine name, manufacturer, serial and batch number, route of administration and location administered; and
- record any adverse reactions to the vaccine and report these to your veterinarian.
Annex 11: Additional guidance on parasite control programs
The frequent use of products (anthelmintics) to control parasites in horses has resulted in increased drug resistance and changes in the parasite populations affecting horses. While large strongyles used to be a significant threat to horses, small strongyles have become widespread and pose greater risk to horses, particularly when significant burdens are found.Footnote 33
Anthelmintic resistance occurs when worms with genetics that provide resistance pass these genes to subsequent generations of worms. As the number of anthelmintic-resistant worms increase, treatments begin to fail.
New strategies are needed to address the changing threats; frequent parasite treatments should be replaced with timed treatments targeting the specific parasites with effective products.
Goals of a parasite control program may include
- Minimizing the risk of parasitic disease;
- Controlling the shedding of parasite eggs and development of infective larvae;
- Minimizing the use of drugs, maintaining effective drugs and preventing or delaying further development of anthelmintic resistance.
ReferenceFootnote 34
Fecal egg count reduction test (FECRT)
Use the FECRT to determine if strongyles and/or roundworms are resistant to a certain anthelmintic. Collect fecal samples prior to deworming and 14 days after the deworming treatment. The percent reduction in eggs can provide an indication of the absence or presence of drug resistance. Use fecal egg count reduction tests at the level of a herd and not the individual horse as they can be quite variable when repeated for a single horse and when performed between horses. For detailed guidance on conducting FECRT, consult your veterinarian and review the Ontario Veterinary Medical Association Proceedings 2014 and American Association of Equine Practitioners Parasite Control Guidelines (2016).
Horses that graze together can demonstrate huge differences in their levels of strongyle egg shedding.
- Within a group of mature horses, strongyle egg counts are highly concentrated in certain horses;
- 20-30% of adult horses usually shed approximately 80% of the eggs.
| Considerations for deworming programs for adult horses: | Considerations for foals, weanling, yearlings |
|---|---|
|
|
General points to consider:
- Ensure correct dosing of horses and do not under-dose horses and foals; use weight tapes or scales to determine body weights.
- Small and large strongyles, and tapeworms are acquired on pasture. Roundworms and pinworms can be acquired in confinement as well as on pasture.
- Have a fecal egg count done on all new arrivals and deworm appropriately before any turnout or sharing a stall.
- Concentrate drug treatments when the local climate favors parasite transmission.
- Design a parasite control program that considers the farm's management practices and region of the country. Consider the following:
- Stocking density: Many horses and/or many different owners may make it more difficult and labor intensive to treat each horse as an individual.
- Heavy stocking rates resulting in a consistently high level of parasite exposure can challenge even the best deworming program.
- Time horses spend on pasture: Limited access or the absence of grass often contributes to low fecal egg counts.
- Age of horses on the farm: Are there foals/weanlings/yearlings and/or mature adults? Treat youngsters as high shedders.
- Is this an "open" herd: Institute a biosecurity program for all new arrivals that includes a fecal egg count and larvicidal deworming prior to turn-out with resident horses. What is the farm's ability or willingness to "clean up" the environment using non-chemical means such as pasture rotation, cross-grazing with other species, manure removal and composting?
Annex 12: Important gastro-intestinal nematode parasites of horses in Canada
| Parasite | Transmission and disease in horse |
|---|---|
| Large strongyles (Strongylus vulgaris, S. edentatus, S. equinus and Triodontophorus) | Eggs shed in manure and develop into larvae in environment. Horses infected by eating larvae on pasture or in bedding. Larvae migrate through abdominal arteries and into other organs. Horses appear unthrifty and weak, may cause diarrhea, weight loss, colic and bleeding. |
| Small strongyles (Cyathostomes – many species). | Eggs shed in manure and develop into larvae. Horses infected by eating larvae on pasture or in bedding. Larvae damage the intestine. Often few clinical signs. Weight loss if heavy burden. |
| Large roundworms (Parascaris equorum) | Eggs shed in manure. Horses infected by eating eggs on pasture or in bedding. Larvae migrate through abdomen to lungs which are coughed up, swallowed and enter the intestine. Respiratory or intestinal signs, unthrifty, weight loss, and colic. |
| Pinworms (Oxyuris equi) | Eggs eaten off of hay or after contact with another horse. Eggs develop into worms in intestinal tract. Worms migrate out of rectum and deposit eggs near anus. Causes irritation of area, itching and hair loss. |
| Lungworms (Dictyocaulus arnfieldi) | More common in donkeys and mules. Eggs or larvae ingested on pasture, in bedding. Larvae migrate through intestine to lymph nodes and lungs where they mature to adult worms. Eggs from adult worms are coughed up, swallowed and enter intestine. Irritation of lungs, coughing, difficulty breathing, can lead to pneumonia. |
| Tapeworms (Anopolocephalus magna, Anopolocephalus perfoliata and Paranoplocephala mammillana) |
Worm segments containing eggs shed in manure. Eggs eaten by pasture mites which are eaten by horses when grazing. Larvae develop in intestinal tract. Can cause irritation of stomach, weight loss and colic. |
| Body cavity worms (Setaria equina) | Adult worms in abdomen produce larvae which enter the blood and can be transmitted to mosquitoes. Larvae mature in mosquitoes and can be transferred to horses when mosquitoes feed. Occasionally adult worms migrate to lungs and infrequently to the eye. Migration to the eye can cause significant inflammation and lead to blindness. |
| Bots (Gasterophilus intestinalus) | Flies lay eggs that stick to horse hair. Larvae develop and are ingested by horse. Cause irritation to mouth and stomach. |
Table Notes
- Table Note 35
-
Bliss DH. The Control of Gastro-Intestinal Nematode Parasites in Horses with Emphasis on Reducing Environmental Contamination. "A New Control Strategy for an Old Problem." MidAmerica Ag Research, Verona, WI.
Annex 13: Separating sick horses
Separating sick horses requires preventing direct contact between horses (for example nose-to-nose contact, social interaction and breeding) and indirect contact with surfaces that may be contaminated (for example, tack, water buckets, hands, clothing, footwear, stall walls, and bedding). Finding sufficient space to separate horses can be difficult.
Housing
Designate a location to house and treat sick horses.
- Select a stall in a separate building that is downwind of the location of the resident horse housing. It should be minimum distance of 25 m from other horses; the farther away the better to prevent aerosol and airborne transmission of pathogens. The building should prevent contact with other horses, be removed from the regular traffic flow on the site and have its own dedicated turn-out area.
- When this is not feasible, consider creating a temporary stall within an outbuilding on the property or use a shed within a paddock. Temporary fencing and portable fence panels can assist with creating the necessary separation. Restrict access to these areas these areas while occupied by an sick horse. To prevent fence line nose-to-nose contact of horses, paddocks on either side of the designated area may need to be left empty.
- While not ideal, sick horses can be managed in the regular housing by moving them to a stall at the end of the barn away from heavy traffic routes and separated from other horses by leaving the adjacent stall empty. Shared airspace and the possible cross contamination by people and equipment reduce the effectiveness of this method. Have dedicated equipment for the sick horse. Install fans near the stall to direct airflow away from the rest of the barn.
- Ideally, the surfaces of the housing area, including the floor, should be non-porous and easy to clean.
- The location should provide the ability to control access to restrict entry and movements of people, vehicles, equipment and horses.
- Post signage advising access to the area is restricted and provide written protocols for entry.
- Either dedicate staff to care only for the sick horses or implement protocols for routine staff to minimize the potential transmission of pathogens to other horses. Create barriers for pathogen transmission by caring for sick horses after the healthy herd and following appropriate protocols such as hand washing and clothing and footwear changes on entering and leaving the area.
- Establish a manure storage area for these horses that is separate from the manure storage used for the healthy horses.
- Stalls and paddocks must be cleaned and disinfected after use for the care and treatment of sick horses.
- Your veterinarian or other sources of biosecurity expertise will be able to advise you on the best practices for separation.
Supplies and equipment
- Dedicate equipment and supplies for the treatment of sick horses that is not shared with other animals. This includes waterers and feeders, water buckets, garbage containers, wheelbarrows, pitchforks, and horse tack (blankets, halters, leads, brushes, and foot picks).
- Identify the equipment for use in this area using coloured paint, tape or a permanent marker.
- Ensure there are handwashing or hand sanitation stations, a boot wash and dedicated outer clothing and boots.
- Stock the necessary medical supplies including medications and thermometer.
| Equipment | Supplies | Miscellaneous |
|---|---|---|
|
|
|
Annex 14: Selected disinfectants
| Active agent | Product examples | Contact time | Advantages | Disadvantages | Comments |
|---|---|---|---|---|---|
| Hypochlorite | Bleach. 1:10-1:50 dilution of household bleach with clean water |
10 min |
|
|
|
| Potassium peroxymonosulfate | Virkon Trifectant |
10 min |
|
|
|
| Accelerated hydrogen peroxide | Accel Peroxigard |
5 - 10 min |
|
|
|
| Quaternary ammoniums | Various | 10-30 min |
|
|
|
| Phenolics | Various | 10 min |
|
|
|
| Alcohol, povidone iodine, chlorhexidine, acids |
|
Product selection and use
Disinfectants are regulated by Health Canada for safety, efficacy and quality when used according to the label directions. However, efficacy is determined under controlled laboratory conditions, and if using disinfectants in a farm environment, they must be used according to the manufacturer's recommendations and considerations given to increased organic load and environmental conditions. Disinfectants are primarily only effective when applied to clean, dry surfaces; their effectiveness is affected by many factors including temperature, pH of the water, presence of other chemicals, concentration and contact time.
As temperatures drop below 10°C, many chemical disinfectants require increased contact time and/or a higher concentration to achieve effective disinfection. Quaternary ammonium compounds are more affected by decreased temperatures than hydrogen peroxide, bleach and potassium peroxymonosulfate. As temperatures approach freezing, disinfection becomes difficult; trailers, equipment and other items should be cleaned and disinfected in a heated building.
Annex 15: Cleaning and disinfecting procedures
The five-step process of cleaning and disinfection
Cleaning and disinfection are two different processes. Cleaning refers to the physical removal of organic material to allow exposure of the object's surface (for example, equipment or stall) to a disinfectant. The cleaning procedure is composed of a dry cleaning and a wet cleaning process. Dry cleaning removes the majority of organic debris (manure, bedding, debris and soil) while wet cleaning helps remove residues and biofilms from the surfaces with the use of hot water and detergents.
Disinfection refers to the application of a disinfectant (often a chemical) to a clean surface to destroy the majority of remaining pathogens. No single disinfectant is adequate for all situations. Disinfection protocols used on a daily basis will differ from those used to control an infectious disease outbreak. However, both disinfection protocols require thorough cleaning and washing prior to the application of any disinfectant.
The full process of cleaning and disinfection involves five steps in the following order:
- Dry cleaning
- Wet cleaning
- Drying
- Disinfection
- Drying
Step 1: Dry cleaning
Begin by moving all horses and other animals out of the areas to be cleaned. Remove any garbage, materials and equipment; remove feed and water buckets/troughs, hay nets, halters and leads, grooming equipment, and anything else that has found a resting place in the area to be cleaned.
Starting at the top of the surface to be cleaned and working down, scrape, knock, brush or wipe off accumulations of organic debris. Work from cleaner to dirtier areas to minimize unnecessary contamination of surfaces. Collect and dispose of organic debris in the manure pile. By thoroughly dry cleaning, the wet cleaning will be easier.
Step 2: Wet cleaning
Using a LOW-PRESSURE SPRAY (to minimize spreading pathogens), wet down surfaces with a solution of warm water and a detergent or degreaser. The detergent/degreaser assists in removing soil, oils and biofilms (colonies of microbes protected by a slimy /mucoid substance). The removal of biofilms is critical to eliminating organisms that may potentially cause disease.
Start by applying the solution to the most heavily contaminated areas and then proceed to apply from the top down. After allowing the solution to fully saturate the organic debris, continue cleaning using a low-pressure spray and warm water: scrub surfaces using brushes and scrapers as necessary. When the surfaces are visibly clean, thoroughly rinse with warm water to remove any remaining detergent and biofilm. Use a squeegee to remove water from floor surfaces to facilitate drying.
Step 3: Drying
Allow the surfaces to thoroughly dry. This assists in destroying the pathogens and minimizes dilution of the disinfectant. Use fans or heaters to speed up the drying process.
Step 4: Disinfection
Select an appropriate disinfectant and prepare it according to the label directions. Protect yourself by wearing appropriate clothing and personal protective equipment (for example, gloves, eye protection, boots and coveralls). Apply the disinfectant to the clean dry surfaces to the point of runoff moving from the top down. Reapply the disinfectant as necessary to ensure the surfaces remain wet for the appropriate contact time specified by the manufacturer. This will usually be a minimum of 10 minutes. Rinse surfaces if required by the manufacturer. Always rinse food and water troughs before refilling.
Step 5: Drying
Allow all surfaces to thoroughly dry before use. Use fans or heaters to speed up the drying process.